Key Facts about Building the Uterine Lining:
-
Successful implantation of the egg is only possible if the uterine lining is sufficiently developed.
-
Estrogens promote the growth of the lining, while progesterone ensures it is maintained.
-
Optimal endometrial thickness ranges between 8 and 14 millimeters.
-
An active lifestyle, healthy nutrition, and stress management can positively influence the thickness of the uterine lining.
-
Fertility supplements containing Coenzyme Q10, Vitamin D3, and Omega-3 support the development of the endometrium.
-
In certain cases, medical treatments such as estrogen therapy may be necessary.
The Uterine Lining: An Often Underestimated Factor in Fertility
When it comes to fertility and the female reproductive system, the focus is usually on aspects like egg quality, hormone levels, or the woman’s age. However, one crucial factor is often overlooked: the uterine lining, medically referred to as the endometrium.
It is just as important as the egg itself in achieving pregnancy. Only when the lining is sufficiently built, well-perfused, and functional can a fertilized egg implant - regardless of how well-developed the embryo is.
But what exactly is the uterine lining, what role does it play in the female cycle - and how can its development be specifically supported?
Why Is the Uterine Lining Important?
The endometrium is the inner lining of the uterus and plays a critical role in the menstrual cycle. It is a tissue that builds up and sheds cyclically, regulated by female hormones - especially estrogen and progesterone. The corpus luteum hormone progesterone helps maintain the developed uterine lining.
Key Functions of the Uterine Lining
-
Preparing for implantation: In the second half of the cycle, the endometrium becomes “receptive” under the influence of progesterone—meaning it becomes ready to receive a fertilized egg.
-
Early nourishment of the embryo: During the first weeks of pregnancy—until the placenta is fully developed—the embryo is nourished via the uterine lining.
-
Immunological protection: The endometrium helps protect the pregnancy and prevents the maternal immune system from rejecting the embryo as a foreign body.
-
Menstruation if no implantation occurs: If implantation doesn’t happen, the top layer of the endometrium is shed and menstruation begins.
Without a sufficiently developed, well-perfused, and hormonally receptive uterine lining, successful implantation - and therefore a healthy pregnancy - is hardly possible. It is a central element in the fertility journey.
How Thick Should the Uterine Lining Be?
The thickness of the lining is an important marker of receptivity. It can be assessed well via ultrasound. Studies show that a thickness between 7 and 14 millimeters in the second half of the cycle offers optimal conditions for implantation (Bu et al., 2016). Values below this (“thin endometrium”) or overly thick linings are associated with lower pregnancy rates. While pregnancies can occur even at 4–5 mm, the likelihood of successful implantation increases significantly above 7 mm (Tomic et al., 2020).
Why Should the Uterine Lining Be Triple-Layered?
A “triple-layered” or trilaminar endometrium is a key sign of a well-prepared, receptive lining ready for implantation. It describes a clear distinction between the endometrial lining, uterine muscle, and cavity. These layers should be well visible via ultrasound right before ovulation. Studies show that a distinct triple-layered appearance correlates with higher implantation and pregnancy success (Zhao et al., 2014).
If this multilayered structure is not visible or the endometrium appears homogenous and undifferentiated, this may indicate reduced receptivity.
Causes of Insufficient Uterine Lining
A thin endometrium can result from various causes including hormonal imbalances, uterine scarring, autoimmune disorders, and polycystic ovary syndrome (PCOS). Common causes include:
-
Hormonal imbalance, especially estrogen deficiency: This can result from age or stress. As women age, estrogen levels drop, and blood vessels in the endometrium become less flexible, hampering regeneration and resulting in thinner linings.
-
PCOS can lead to elevated androgen levels that disrupt ovulation and impair endometrial development.
-
Impaired uterine blood flow: Poor blood flow can lead to a thinner lining. Contributing factors include smoking, obesity, hypertension, diabetes, or use of hormonal contraceptives. Measures like reducing cholesterol, avoiding long periods of sitting, and regular exercise can help.
-
Chronic endometritis: Postpartum inflammation can result in a persistently thin endometrium visible on ultrasound.
-
Autoimmune diseases: Conditions like celiac disease, Crohn's disease, or rheumatoid arthritis may affect endometrial health.
-
Adhesions or scarring: May occur after curettage or infections (STDs), leading to thinning.
-
Clomiphene citrate: Used to stimulate ovulation, but may thin the uterine lining as a side effect.
-
Underweight or malnutrition: Inadequate nutrition can cause the body to break down muscle, including uterine muscle, resulting in a thinner lining.
Symptoms of a Thin Uterine Lining
A thin endometrium typically causes no noticeable symptoms and often goes undetected. Occasionally, menstruation may be very light or irregular.
What Can Help Build the Uterine Lining?
1. Lifestyle, Nutrition, and Stress Reduction
An active lifestyle benefits general health and improves endometrial development. Sedentary habits slow blood flow. Regular light exercise boosts pelvic circulation, bringing more oxygen and nutrients to the endometrium.
A nutrient-rich, balanced diet strengthens the endometrium with essential minerals. Foods like leafy greens, legumes, whole grains, berries, nuts, seeds, and omega-3-rich fish support cellular health and lining growth.
Reducing stress is also essential: chronic stress disrupts hormonal balance, especially estrogen and progesterone, which are vital for a healthy lining. Relaxation techniques can help reduce stress and create favorable conditions for the endometrium.
2. Micronutrients Supporting the Uterine Lining
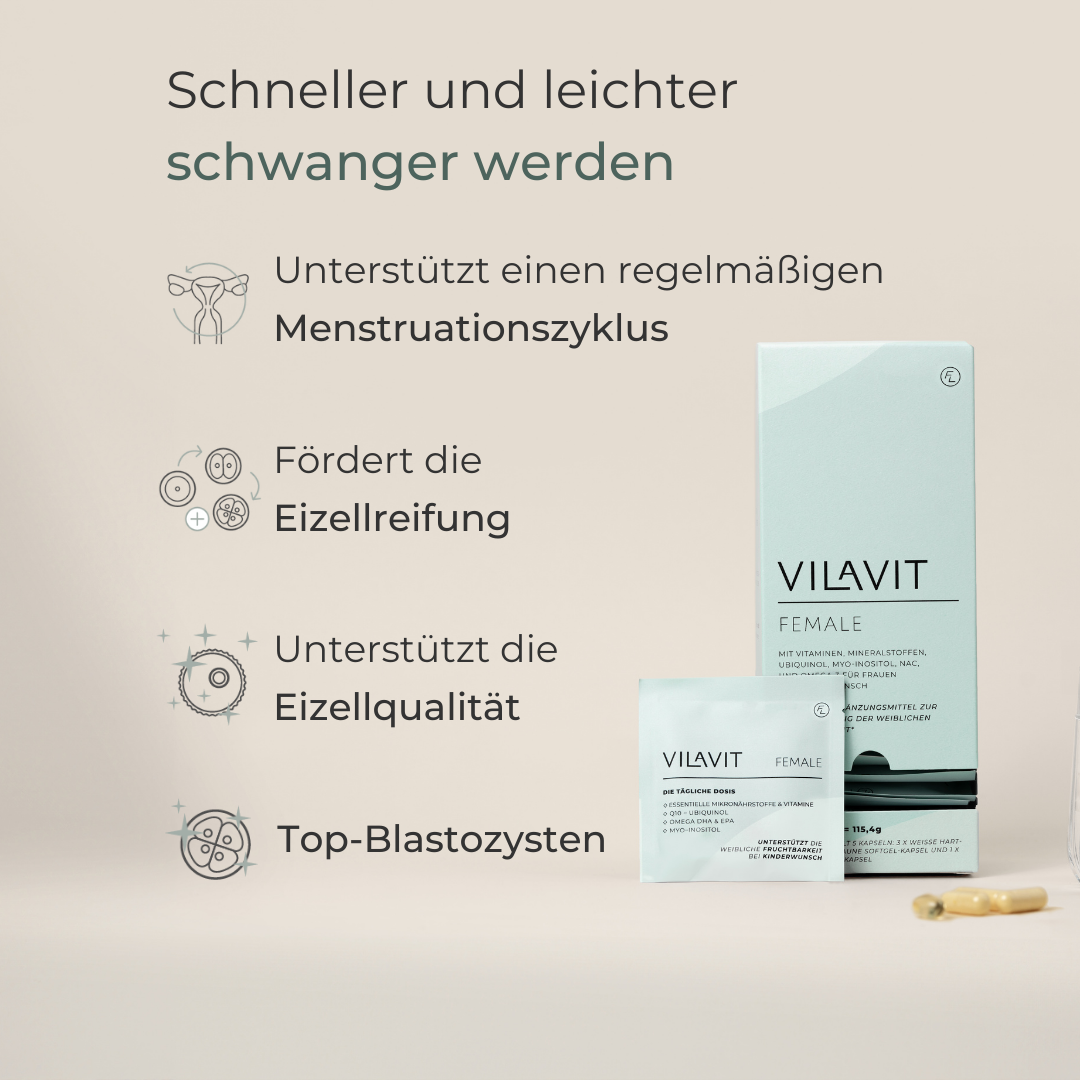
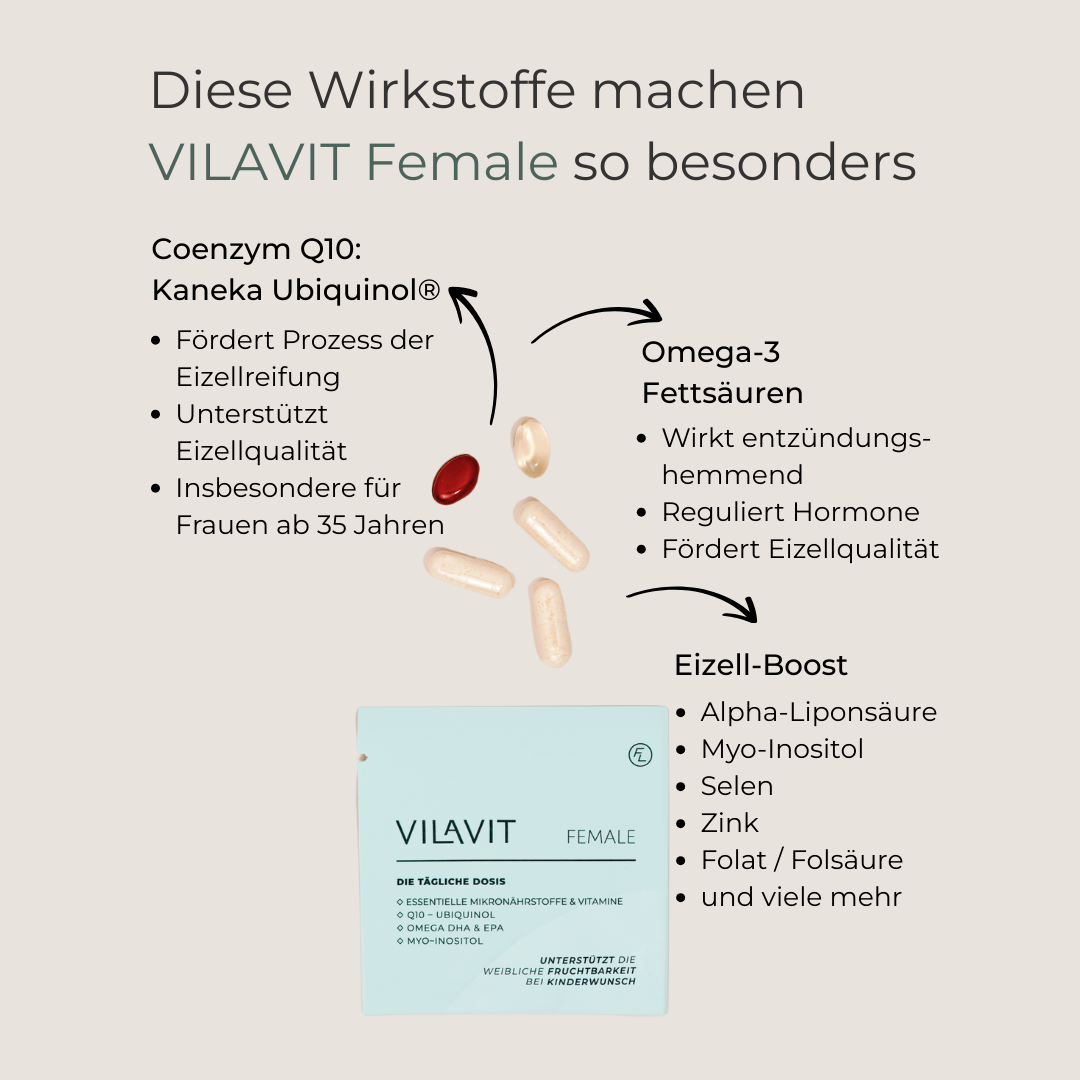
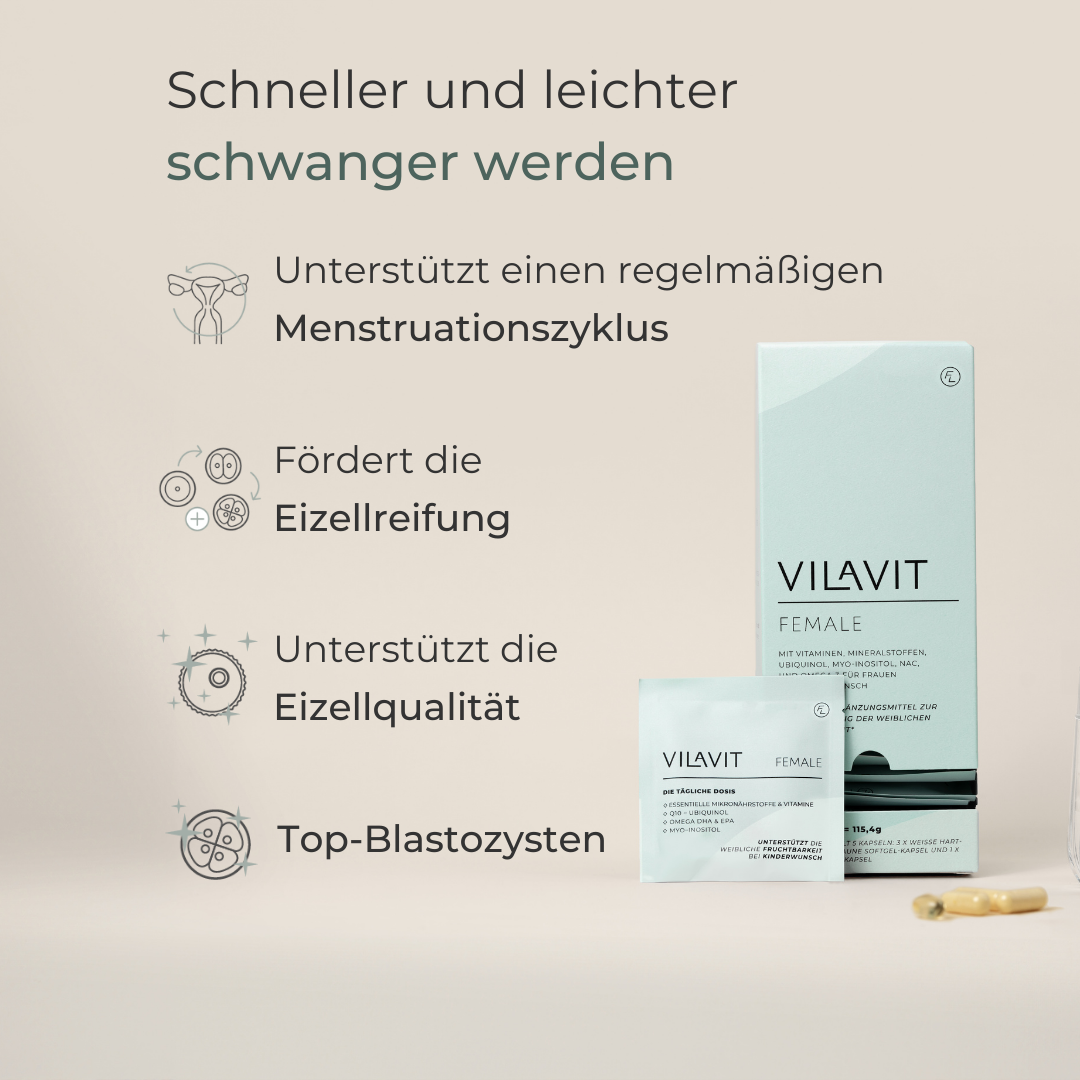
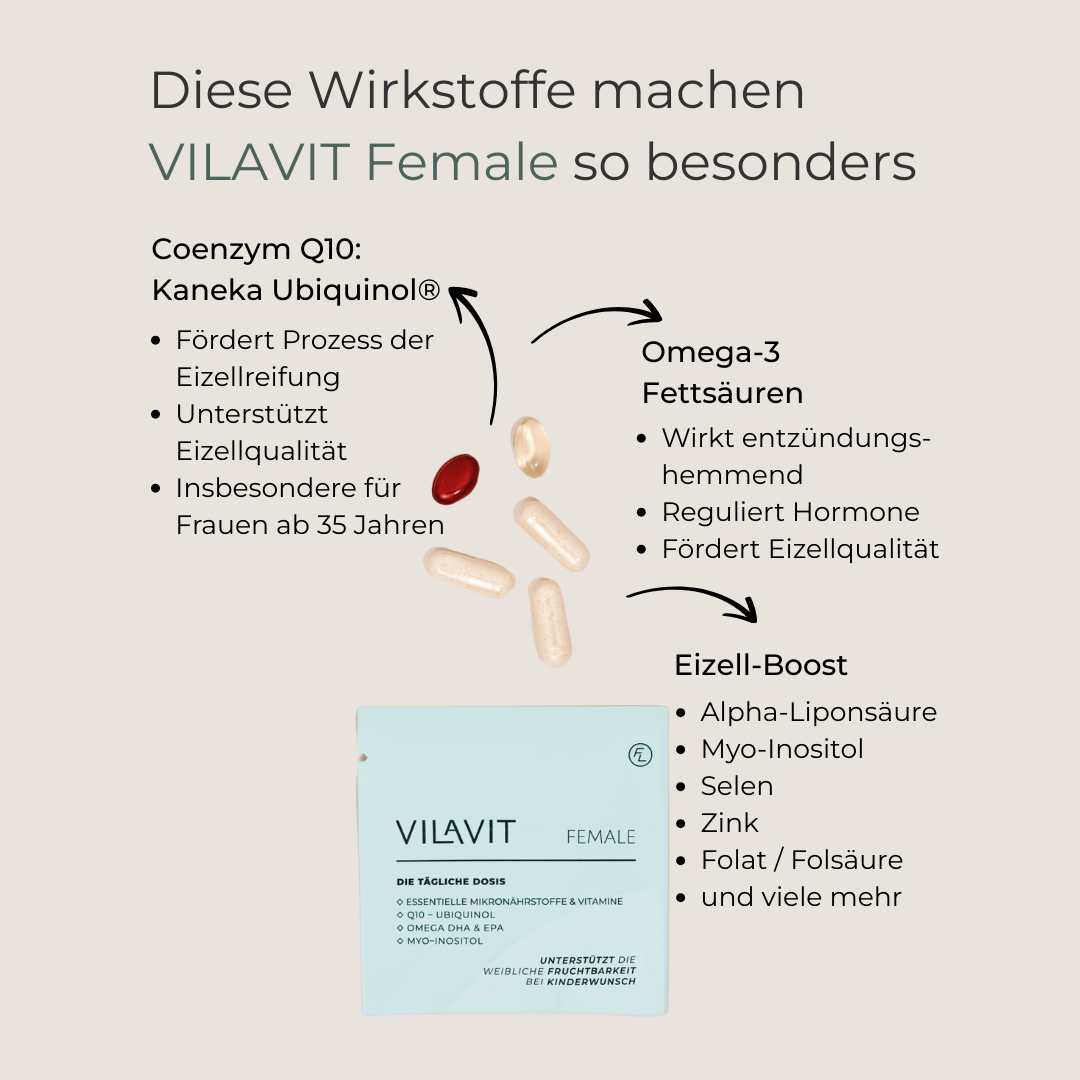
Certain nutrients - like those in VILAVIT Female - support cellular development of the endometrium:
-
Coenzyme Q10: In its active form ubiquinol, supports cell division and tissue development. Studies show it can improve endometrial thickness (El Refaeey et al., 2014).
-
Omega-3 fatty acids: Omega-3 fatty acids have anti-inflammatory effects. They strengthen the uterine lining and reduce uterine inflammation, enhancing pregnancy chances (Trop Steinberg et al., 2024).
-
Vitamin D: Adequate levels are associated with a healthier, better-developed endometrial lining (Arabian et al., 2018).
3. Acupuncture to Improve Blood Flow
Acupuncture can enhance uterine blood flow and improve the trilaminar pattern of the endometrium (Zhong et al., 2019). It is often used alongside IVF treatments.
4. PRP Therapy (Platelet-Rich Plasma)
For women with a thin lining, PRP offers a promising new option. It is derived from the patient’s own blood and is rich in platelets and growth factors that promote cellular growth and angiogenesis. PRP is injected directly into the uterus, with positive effects often visible after two to three cycles (Chen et al., 2024).
5. Estrogen Therapy
Estrogen therapy can help thicken the endometrium via patches, gels, or oral/vaginal tablets. Studies confirm it improves endometrial thickness and implantation rates (Chen et al., 2006).
Conclusion: The Uterine Lining Is Key When Trying to Conceive
The endometrium is vital for embryo implantation and a healthy pregnancy. Women trying to conceive should pay special attention to its development. Whether through a healthy lifestyle, targeted micronutrients, hormonal support, or alternative methods - many strategies exist to help the body create optimal conditions for successful implantation.
FAQs: Building the Uterine Lining
Do alternative approaches like chaste tree berry or raspberry leaf tea help build the uterine lining?
Chaste tree berry may support hormonal balance, but there is no conclusive evidence that it directly enhances endometrial development. Likewise, raspberry leaf tea has not been scientifically proven to impact lining thickness or function.
Can I undergo fertility treatment with a thin uterine lining?
It is essential to work with fertility specialists to identify the underlying cause of a thin lining and determine the best treatment approach.
How does the EMMA Receptivity Test help in cases of thin uterine lining?
The EMMA test does not assess thickness or structure but evaluates the lining’s receptivity at cellular and immunological levels. This can still provide valuable insights—even when the lining is thin.
References
-
Bu, Z., Wang, K., Dai, W., & Sun, Y. (2016). Endometrial thickness significantly affects clinical pregnancy and live birth rates in frozen-thawed embryo transfer cycles. Gynecological Endocrinology, 32(7), 524–528. https://doi.org/10.3109/09513590.2015.1136616
-
Tomic V, Kasum M, Vucic K. Impact of embryo quality and endometrial thickness on implantation in natural cycle IVF. Arch Gynecol Obstet. 2020 https://link.springer.com/article/10.1007/s00404-020-05507-
-
Zhao J, Zhang Q, Wang Y, Li Y. Endometrial pattern, thickness and growth in predicting pregnancy outcome following 3319 IVF cycle. Reprod Biomed Online. 2014 https://pubmed.ncbi.nlm.nih.gov/25070912/
-
Chen MJ, Yang JH, Peng FH, Chen SU, Ho HN, Yang YS. Extended estrogen administration for women with thin endometrium in frozen-thawed in-vitro fertilization programs. J Assist Reprod Genet. 2006 https://pubmed.ncbi.nlm.nih.gov/16983519/
-
Shivtia Trop-Steinberg, Michael Gal, Yehudith Azar, Rachel Kilav-Levin, Eliyahu M. Heifetz, Effect of omega-3 supplements or diets on fertility in women: A meta-analysis, Heliyon, 2024 https://doi.org/10.1016/j.heliyon.2024.e29324
-
Arabian S, Raoofi Z. Effect of serum vitamin D level on endometrial thickness and parameters of follicle growth in infertile women undergoing induction of ovulation. J Obstet Gynaecol. 2018 https://www.tandfonline.com/doi/full/10.1080/01443615.2017.141189
-
Zhong Y, Zeng F, Liu W, Ma J, Guan Y, Song Y. Acupuncture in improving endometrial receptivity: a systematic review and meta-analysis. BMC Complement Altern Med. 2019 https://bmccomplementmedtherapies.biomedcentral.com/articles/10.1186/s12906-019-2472-1
-
Po-Fan Chen, Yu-Ling Liang, Yuan-Jhe Chuang, Meng-Hsing Wu, Autologous PRP therapy for thin endometrium: A self-controlled case series study across menstrual cycles, European Journal of Obstetrics & Gynecology and Reproductive Biology, Volume 299, 2024 https://doi.org/10.1016/j.ejogrb.2024.05.032