The most important things to know about fertility and PCOS at a glance:
- About 5-10% of women of reproductive age are affected by PCOS.
- PCOS leads to increased male hormones (androgens) and disrupts the female cycle.
- Genetics, hormones, and environmental factors likely play a role together.
- Common symptoms include irregular cycles, acne, excess body hair, hair loss, weight problems, and insulin resistance.
- A healthy diet, exercise, and weight loss can improve the chances of getting pregnant.
How to get pregnant with PCOS
Polycystic Ovary Syndrome (PCOS) is a common hormonal disorder that significantly affects fertility and can make it difficult to get pregnant or fulfill the desire to have children. Women affected by PCOS often experience infertility due to the lack of regular ovulation.
Despite the challenges that come with PCOS, there are now numerous evidence-based approaches that can help reduce the impact of PCOS on fertility and improve the chances of pregnancy. Fertility clinics offer specialized fertility treatments, ranging from hormone therapy to assisted reproduction, such as intrauterine insemination (IUI) or in-vitro fertilization (IVF).
Learn everything important about the most common causes and diagnosis of PCOS, as well as proven therapy approaches. We also provide valuable tips on how to improve your chances of getting pregnant.
What is Polycystic Ovary Syndrome (PCOS)?
Polycystic Ovary Syndrome (PCOS) is a complex metabolic disorder (endocrine disorder) characterized by a number of symptoms. It is considered one of the most common hormonal disorders in women and affects about 5-10% of women of reproductive age.
With polycystic ovary syndrome, the body produces more male sex hormones (androgens). This leads to improper regulation of the menstrual cycle. The follicles in the ovaries do not mature properly, causing women with PCOS to often not have regular ovulation. The lack of maturation and release of eggs impairs fertility in affected women.
One aspect of PCOS can be the presence of polycystic ovaries. This means that many small, fluid-filled sacs develop in the ovaries, visible on ultrasound. However, PCOS is a complex hormonal disorder that goes beyond these cysts.

Diagnosis of PCOS
The diagnosis of polycystic ovary syndrome (PCOS) is made through a combination of blood tests to check hormone levels, ultrasound scans, and medical consultations about the presence of certain symptoms. To get a comprehensive diagnosis and treatment, you should schedule an appointment with your gynecologist or a fertility clinic.
The key steps in diagnosing PCOS include:
-
Blood tests A blood test helps check the hormones in the blood and establish hormone levels. Key hormones include:
- Androgens: Elevated androgen levels in the blood (hyperandrogenemia), such as testosterone and dihydrotestosterone (DHT), can be an indicator of PCOS.
- Testosterone: >70 ng/dl is elevated, >100 ng/dl is highly elevated.
- Dihydrotestosterone (DHT): >150 ng/dl.
- Luteinizing hormone (LH) and follicle-stimulating hormone (FSH): A common pattern in PCOS is an increased ratio of luteinizing hormone to follicle-stimulating hormone. While LH is often elevated, FSH levels may be normal or low. A ratio of LH to FSH of 2:1 or higher may indicate a hormonal imbalance.
- Progesterone and estrogen: In PCOS, the ratio of progesterone to estrogen is often disrupted. Many cases show estrogen dominance. This doesn’t necessarily mean the estrogen level is absolutely elevated, but there is an imbalance compared to progesterone. Due to the often irregular or absent ovulation in PCOS, too little progesterone (a progestogen) is produced in the second half of the cycle.
- Insulin: Since many women with PCOS have insulin resistance, insulin levels can also be elevated. Elevated fasting insulin or impaired glucose metabolism can indicate insulin resistance.
- SHBG (Sex hormone-binding globulin): In PCOS, SHBG levels are often too low. SHBG binds testosterone and other androgens, and lower levels can lead to higher free androgen levels in the blood.
-
Transvaginal ultrasound An ultrasound of the ovaries is performed to check for the presence of numerous small egg sacs in the ovaries. This is a characteristic but not sufficient feature for diagnosing PCOS.
-
Medical consultation (Anamnesis) Based on your blood values and the ultrasound, your doctor can gain a better understanding of your cycle and provide an assessment. In a consultation with a specialist, you will be asked about the following symptoms of PCOS:
- Irregular menstrual cycles: Infrequent menstruation (oligomenorrhea) or absence of menstruation (amenorrhea).
- Excess body hair (hirsutism).
- Acne.
- Hair loss.
- Medical/family predisposition.
The diagnosis of PCOS is usually based on the Amsterdam criteria. At least two of the following three criteria must be met (Kostroun, 2022):
- Irregular menstruation (9 or fewer periods in 12 months).
- Elevated androgen levels
- The presence of polycystic ovaries (at least 12 follicles of 2-9 mm in at least one ovary).
Causes of PCOS
The exact cause of polycystic ovary syndrome (PCOS) is not fully understood. It is believed that a combination of genetic, hormonal, and environmental factors plays a role.
A possible trigger for PCOS could be a malfunction of an enzyme that normally regulates the production of male hormones. This malfunction leads to an elevated level of androgens, or male hormones, in the body. Such an increase can contribute to the typical symptoms of PCOS, such as irregular menstrual cycles and excessive hair growth.
Symptoms of PCOS
Women with polycystic ovary syndrome (PCOS) may experience a wide range of symptoms. The most common include:
- Irregular menstrual cycles: Very long and irregular cycles or absent periods are a common symptom.
- Ovulation disorders: Lack of regular maturation and release of eggs. This can lead to fertility problems.
- Elevated androgen levels: This can manifest as acne, excessive hair growth (hirsutism), hair loss on the head, or oily skin.
- Polycystic ovaries: Many small cysts may be visible in the ovaries on ultrasound.
- Weight gain: Women with PCOS often have difficulty controlling their weight or are more prone to weight gain.
- Insulin resistance: PCOS can result in insulin resistance, leading to higher blood sugar levels and an increased risk of developing type 2 diabetes.
- Metabolic syndrome: Women with PCOS are at a higher risk for metabolic syndrome, which is characterized by a combination of insulin resistance, overweight, high blood pressure, and elevated blood fat levels. Metabolic syndrome increases the risk of cardiovascular disease and diabetes. A healthy lifestyle with a balanced diet and regular exercise is especially important for women with PCOS.
- Psychological stress: Studies have found that women with PCOS are more likely to suffer from mild to severe depression than women without PCOS. They are also more likely to experience moderate anxiety and stress. (Sulaiman, 2017).
The severity of these symptoms can vary, and not all women with PCOS experience all of these complaints.
Treatment options for PCOS for women trying to conceive
For women with PCOS who are having difficulty getting pregnant, several treatment options are available, aimed at regulating hormone levels.
-
Hormonal stimulation for egg maturation and ovulation induction
- Clomiphene: Stimulates the ovaries to mature eggs and is often used to induce ovulation (ovulation induction) and improve fertility. (Elkhateeb RR. et al, 2017).
- Gonadotropins (LH, FSH, and combination of LH and FSH): Hormones typically used for hormonal stimulation of ovulation in women with polycystic ovary syndrome (PCOS), especially when other treatments like clomiphene citrate are not successful.
-
Supporting measures to improve insulin resistance and metabolism
- Metformin: A medication primarily used to treat type 2 diabetes but can also help improve insulin sensitivity and regulate the menstrual cycle in women with PCOS. However, it's important to note that metformin does not replace the need for lifestyle changes in overweight and obese women with PCOS. (Lashen H. et al, 2018).
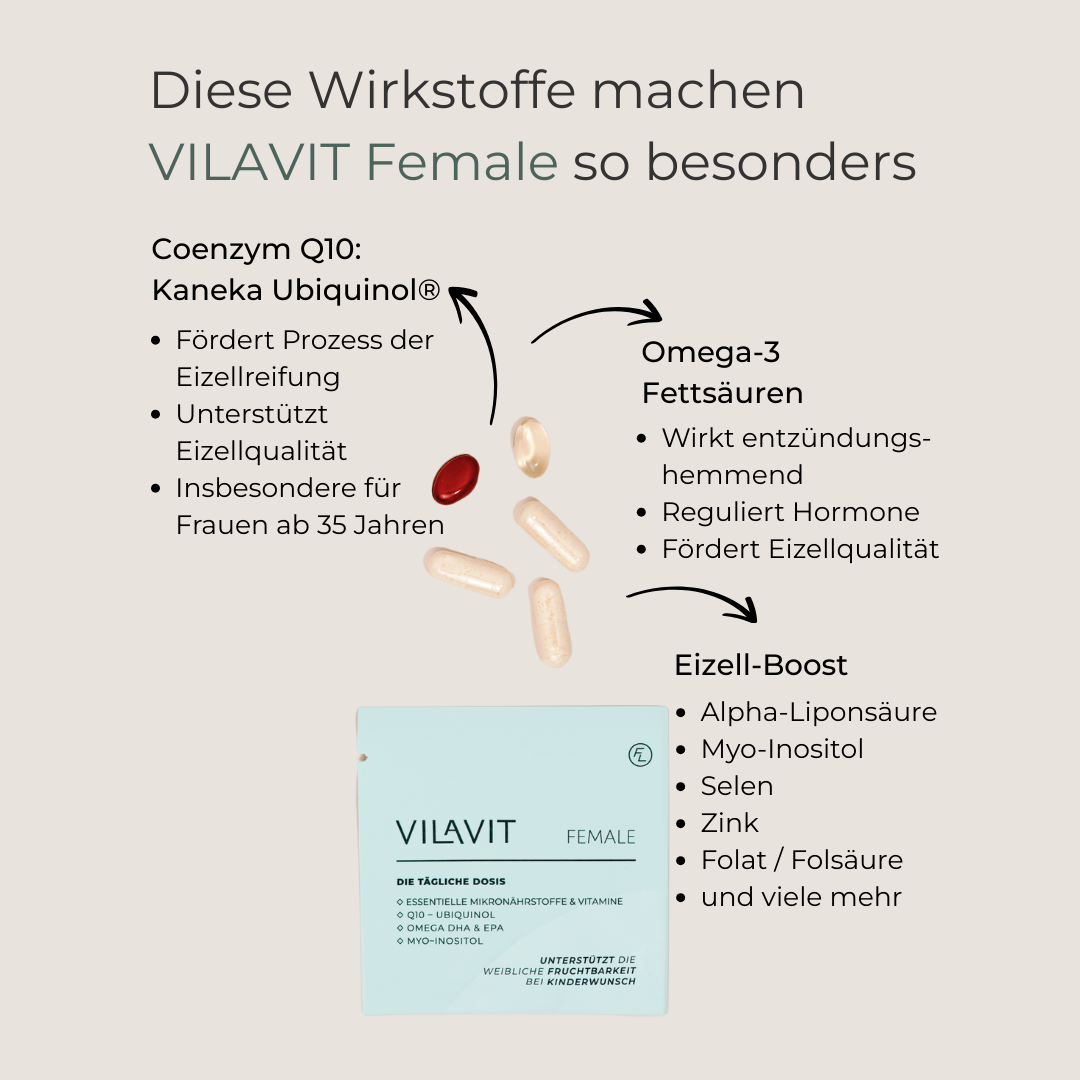
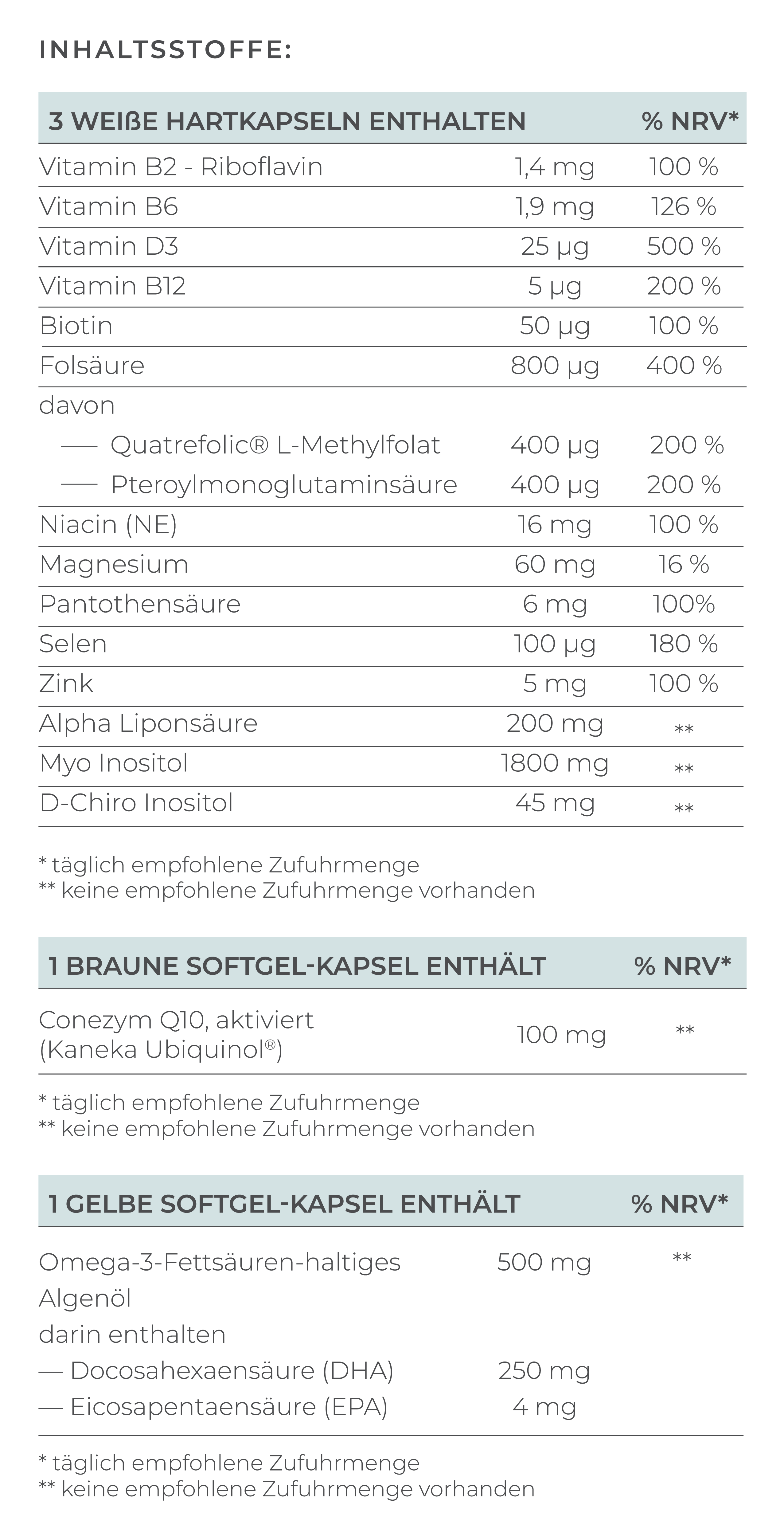
- Myo-Inositol: Improves insulin sensitivity and supports normal ovarian function, which can help regulate the menstrual cycle. (Unfer V. et al, 2017).
-
Further measures
- In-vitro fertilization (IVF): If other treatments have not been successful, fertility treatments can bring you closer to your desired child. During IVF or ICSI, eggs are retrieved, fertilized outside the body, and then implanted into the uterus.
- Laparoscopic ovarian drilling (LOD): A surgical method where small holes are made in the ovaries to reduce androgen production and promote ovulation.
- Hormonal contraception: Birth control pills can help regulate hormone levels and alleviate typical PCOS symptoms, such as acne and excessive hair growth. However, it is not a solution for women trying to conceive.
Tips for women with PCOS trying to conceive
For women with polycystic ovary syndrome (PCOS), the path to pregnancy can be challenging, but there are several effective strategies to improve fertility and increase the chances of a successful conception. Here are some comprehensive tips to help mitigate the effects of PCOS on fertility:
Active Lifestyle
Ensure you get at least 150 minutes of moderate physical activity each week, whether it's brisk walking, cycling, or swimming. Regular exercise helps improve insulin resistance and can contribute to stabilizing your menstrual cycle.
Healthy Diet
Focus on a diet rich in fiber, healthy fats, and lean protein. Avoid highly processed foods and sugar, as these can cause insulin spikes. Instead, opt for whole grains, fresh fruits, vegetables, nuts, and seeds. This diet supports not only your hormone balance but also promotes healthy ovarian function.
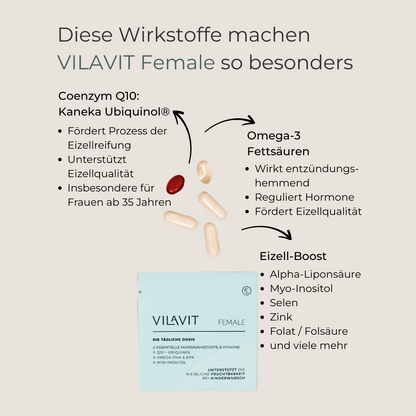
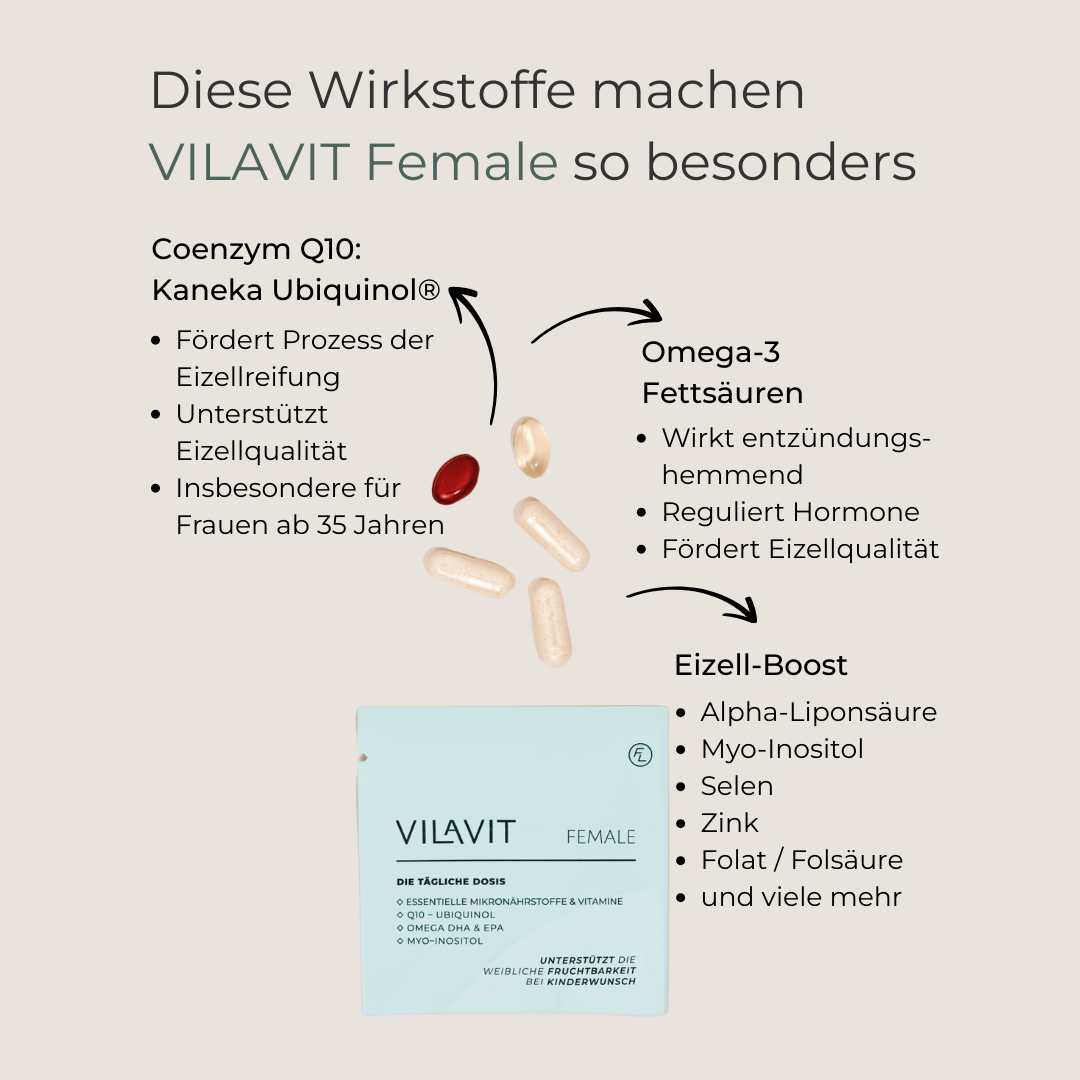
Micronutrients
Incorporate high-quality micronutrients to support healthy ovarian function with regular menstrual cycles, promote ovulation, and improve egg quality.
Weight Loss
If overweight, even a small weight loss of 5-10% can improve insulin resistance, regulate hormone levels, and increase the chances of ovulation.
Medical Support
Consult your specialist for personalized treatment options to boost your fertility.
Use these tips as a foundation to fulfill your desire for a child. By combining lifestyle changes, targeted micronutrients, and informed medical treatment, you can significantly improve your chances of a successful conception. You can do it – stay persistent and be patient with yourself!
Conclusion: The right treatment helps many women with PCOS achieve their dream of having a child
It’s completely normal to feel overwhelmed when you first receive a PCOS diagnosis—especially when you're trying to have a baby. PCOS is a common hormonal disorder that can affect your fertility, but it doesn't mean the end of your journey to parenthood. With the right treatment and a few changes in your daily life, you can greatly improve your chances of getting pregnant.
It’s best to seek support early on from your gynecologist or a fertility clinic. They can provide information on the treatment options available and what will work best for you.
FAQ:
What are the chances of getting pregnant with PCOS?
The chances of getting pregnant with polycystic ovary syndrome (PCOS) vary significantly depending on several factors, including the severity of the syndrome and individual symptoms.
The spontaneous pregnancy rate (without treatment) in PCOS is indeed lower than in women without PCOS. Studies show that about 20-40% of PCOS patients become pregnant spontaneously within a year, compared to 70-80% in women without PCOS (Teede, 2018).
Women with PCOS who receive medical treatment have significantly better chances. For example, the cumulative pregnancy rate after 6 cycles of treatment with metformin and/or clomiphene is about 40-46% (Legro, 2007).
How long does it usually take for a woman with PCOS to get pregnant?
The time to pregnancy can vary because the menstrual cycle in PCOS is often irregular, making it harder to determine the fertile window. However, with appropriate treatment (e.g., hormonal stimulation combined with cycle monitoring), many women can become pregnant within 12 months, but it depends on individual factors.
Do you have to be overweight to be diagnosed with PCOS?
No, you do not have to be overweight to be diagnosed with polycystic ovary syndrome (PCOS). PCOS can occur in women of all weight categories. While being overweight and obesity are common symptoms of PCOS, especially due to the often associated insulin resistance, this is not the only way the syndrome can manifest.
References
- Kostroun et al. Impact of updated international diagnostic criteria for the diagnosis of polycystic ovary syndrome. F & Reports. 2022.
- Elkhateeb RR, Mahran AE, Kamel HH. Long-term use of clomiphene citrate in induction of ovulation in PCO patients with clomiphene citrate resistance. J Gynecol Obstet Hum Reprod. 2017.
- Attia GM, Almouteri MM, Alnakhli FT. Role of Metformin in Polycystic Ovary Syndrome (PCOS)-Related Infertility. 2023.
- Lashen H. Role of metformin in the management of polycystic ovary syndrome. Ther Adv Endocrinol Metab. 2010.
- Unfer V, Facchinetti F, Orrù B, Giordani B, Nestler J. Myo-inositol effects in women with PCOS: a meta-analysis of randomized controlled trials. Endocr Connect. 2017.
- Teede et al. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Fertility and Sterility, 2018.
- Legro et al. Clomiphene, Metformin, or Both for Infertility in the Polycystic Ovary Syndrome. The New England Journal of Medicine, 2007.
- Sulaiman et. al. Psychological burden among women with polycystic ovarian syndrome in Oman: a case–control study. International Journal of Women's Health, 2017.