Everything you need to know about the IVF procedure at a glance
- In IVF, eggs are fertilized with sperm outside the body and then implanted in the uterus.
- If sperm quality is limited, ICSI may be necessary, in which a single sperm is injected directly into the egg.
- The pregnancy rate per IVF cycle is 20-30%, but is strongly age-dependent.
- After several IVF attempts, the cumulative success rate increases significantly - up to 60-70% after three cycles.
- Nutrition, micronutrients and lifestyle have an influence on IVF success.
What to expect from IVF
In vitro fertilization (IVF) is one of the best-known methods of assisted reproductive medicine and offers many couples and single women the chance to fulfil their desire to have children if they are unable to conceive naturally. The IVF process involves several carefully planned steps, which we explain in this article - so that you know exactly what to expect and how the treatment works.
What is in vitro fertilization?
IVF is a form of assisted fertilization in which eggs are retrieved from a woman's body as part of a follicular puncture and fertilized with sperm outside the body in the laboratory. The resulting embryos are then implanted into the woman's uterus with the aim of implantation and pregnancy.
How does IVF work?
IVF involves several steps: Hormonal stimulation of the ovaries, egg retrieval (follicular puncture), sperm retrieval, fertilization in the laboratory, embryo cultivation, embryo transfer to the uterus and finally a pregnancy test.
Here is the exact procedure for IVF:
- Stimulation of the ovaries:
The actual hormonal stimulation of the ovaries is triggered by administering certain medications containing follicle-stimulating hormone (FSH). At the same time, natural premature ovulation is suppressed with medication known as GnRH analogs. The timing of this treatment is determined individually by the treating doctor in order to create optimal conditions for the retrieval of the eggs. As a rule, stimulation lasts 8 to 14 days and involves daily injections.
Two types of medication are generally used:
- FSH or HMG preparations: these contain follicle-stimulating hormones (e.g. follitropin alfa or menotropin), which promote the growth of several follicles in the ovaries.
- GnRH analogs or antagonists: These active substances prevent premature ovulation by specifically blocking the release of the body's own hormones (LH).
The aim of this combined hormone treatment is to allow as many fertile eggs as possible to mature in a controlled cycle.
- Follicular puncture:
The optimum time to retrieve the eggs is determined by ultrasound and blood tests.
As soon as the eggs have matured sufficiently, ovulation is induced with medication (usually with hCG or a GnRH analog). Around 36 hours later, the eggs are retrieved under light anesthesia or sedation. A fine needle is used to aspirate the follicular fluid from the ovaries via the vagina - this contains the mature eggs. The procedure takes around 15 to 20 minutes and is minimally invasive.
On average, 8 to 15 eggs are retrieved, depending on age, hormonal status and response to stimulation.
- Sperm retrieval and preparation:
The man's sperm cells are usually obtained through ejaculation. In the case of limited sperm quality or special medical conditions, a testicular biopsy (TESE) or aspiration from the epididymis (MESA) may be necessary. The sperm is then processed in the laboratory.
- Fertilization:
The retrieved eggs are combined with the prepared sperm in the laboratory. If the sperm quality is limited, an ICSI (intracytoplasmic sperm injection) can be performed, in which a single sperm is injected directly into the egg.
- Cultivation of the embryos:
The fertilized eggs are monitored and further cultured in the incubator. After 3 to 5 days, one or more embryos have developed. The quality of the embryos is assessed regularly. Optionally, the embryos can be genetically tested (pre-implantation genetic diagnosis) before implantation.
- Embryo transfer:
In an IVF cycle, a single embryo is usually transferred into the woman's uterus. The embryo with the best development is gently transferred using a flexible catheter under ultrasound guidance. The process is painless and only takes a few minutes.
Remaining, high-quality embryos can be frozen (cryopreserved) and are available for a later attempt if a further transfer is desired or necessary.
If desired and medically justifiable, several embryos can also be transferred at the same time in order to increase the chances of pregnancy. However, careful consideration is given to minimize the risks of a multiple pregnancy.
Progesterone is administered to support the uterine lining and the implantation of the embryo.
- Pregnancy test:
A blood test (beta-hCG) can be carried out around 14 days after the puncture to determine whether implantation has taken place and a pregnancy exists.
Chances of success of IVF: 20-30% per cycle
The chances of success of in vitro fertilization (IVF) depend largely on the woman's age and individual medical factors. On average, the pregnancy rate per treatment cycle is between 20% and 30%.
- Women under the age of 35 have the highest chances of becoming pregnant with IVF - according to the German IVF Register (DIR), the clinical pregnancy rate in 2022 was around 34% per embryo transfer in this age group.
- Between the ages of 35 and 40, the success rate drops to around 20-25% per cycle.
- From the age of 40, the probability decreases significantly: only around 10-15% of treatments result in pregnancy.
- From the age of 43, studies show that the success rate is less than 5% - in certain cases, egg donation can be considered.
How often does the first IVF work?
The average chance of success for the first IVF treatment is around 25 to 30% - provided the woman is under 35 years old and there are no serious medical restrictions.
It is important to know that pregnancy often does not occur on the first attempt. The cumulative success rate - i.e. the chance of becoming pregnant after several IVF cycles - is significantly higher. Studies show that up to 60-70% of women become pregnant after three complete IVF cycles.
When can IVF be useful?
IVF is necessary if natural fertilization is difficult or impossible - for example due to hormonal disorders, a limited egg reserve, changes in the fallopian tubes or reduced sperm quality.
Reasons for IVF treatment at a glance:
Female causes:
- Reduced ovarian reserve: a low number of eggs or reduced egg quality - often age-related.
- Advanced age: Fertility decreases significantly with increasing age, especially from the age of 35.
- Hormonal disorders: Cycle disorders, anovulation (no ovulation) or hormonal irregularities can prevent fertilization.
- Changes in the uterus: polyps, fibroids or endometriosis can make it difficult for the embryo to implant.
- Fallopian tube problems: Adhesions or blockages in the fallopian tubes make natural fertilization impossible.
- Cervical factor: Changes in the cervical mucus or structural abnormalities can hinder the penetration of sperm.
Male causes:
- Oligozoospermia: Too few sperm in the ejaculate.
- Asthenozoospermia: Limited sperm motility.
- Teratozoospermia: High proportion of malformed sperm.
- Cryptozoospermia: Very few sperm detectable in the ejaculate.
- Oligoasthenoteratozoospermia (OAT syndrome): Combination of low sperm count, poor motility and abnormal morphology.
In some couples, the cause of involuntary childlessness remains unclear - this is referred to as idiopathic infertility. IVF can also be useful in such cases.
How can the right diet support IVF?
A balanced diet plays an important role in fertility and the chances of success of IVF treatment. Studies show that certain micronutrients and foods can have a positive effect on egg quality, hormone balance and the uterine lining.
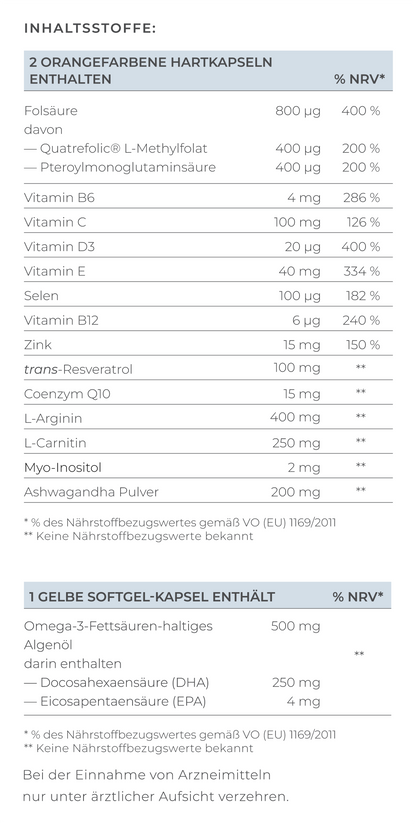
Important nutrients
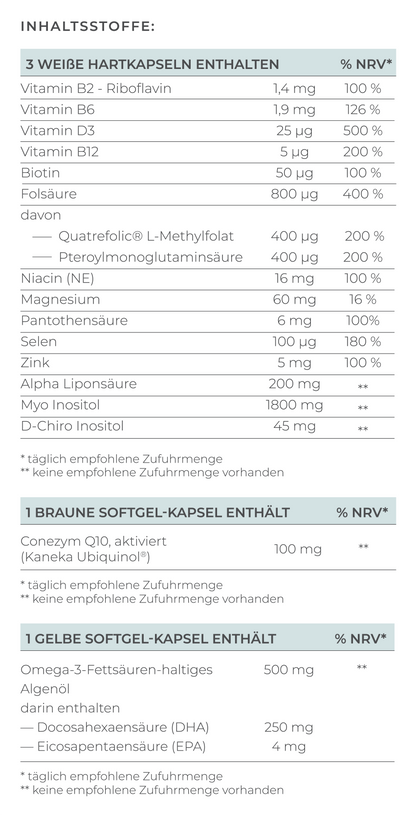
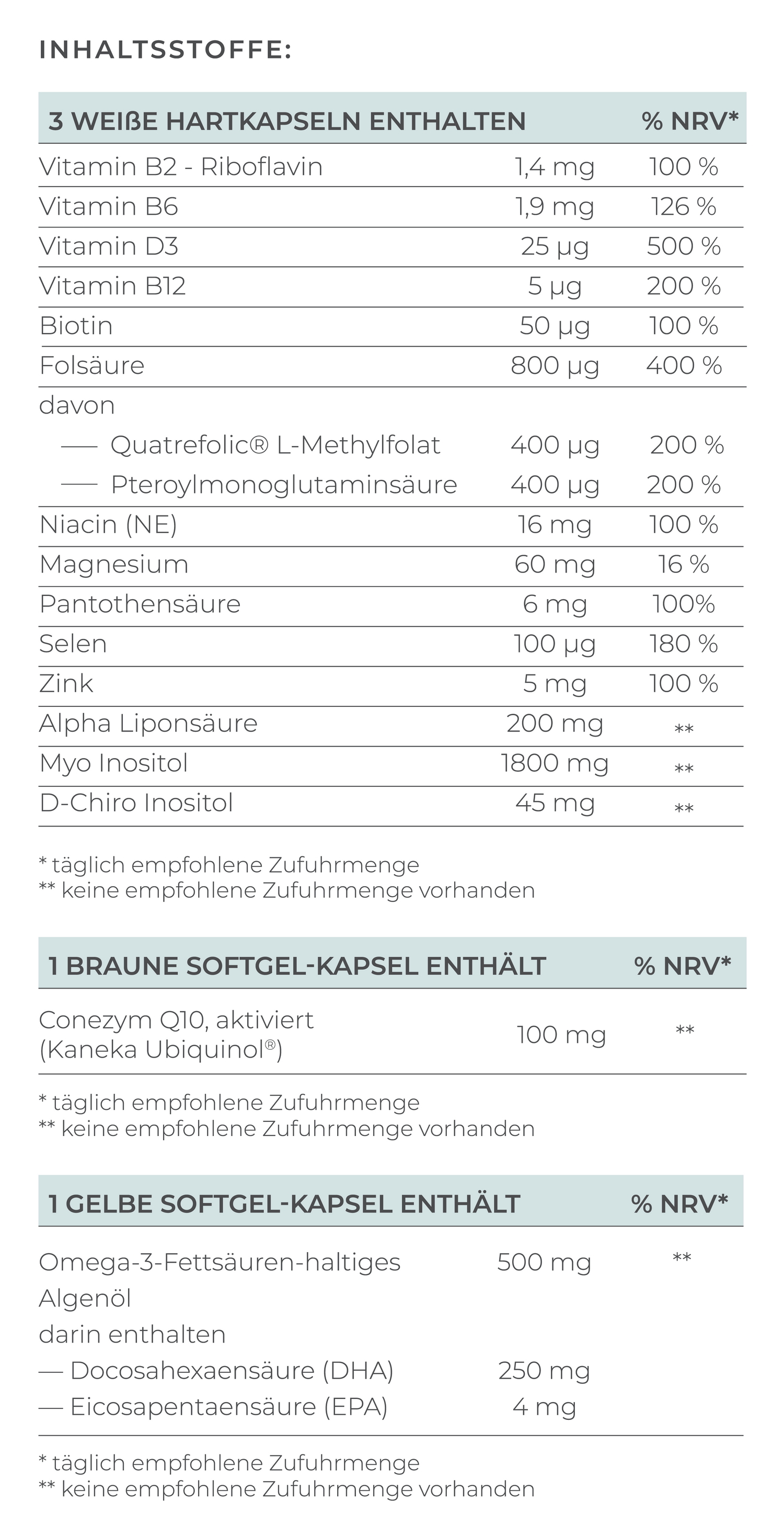
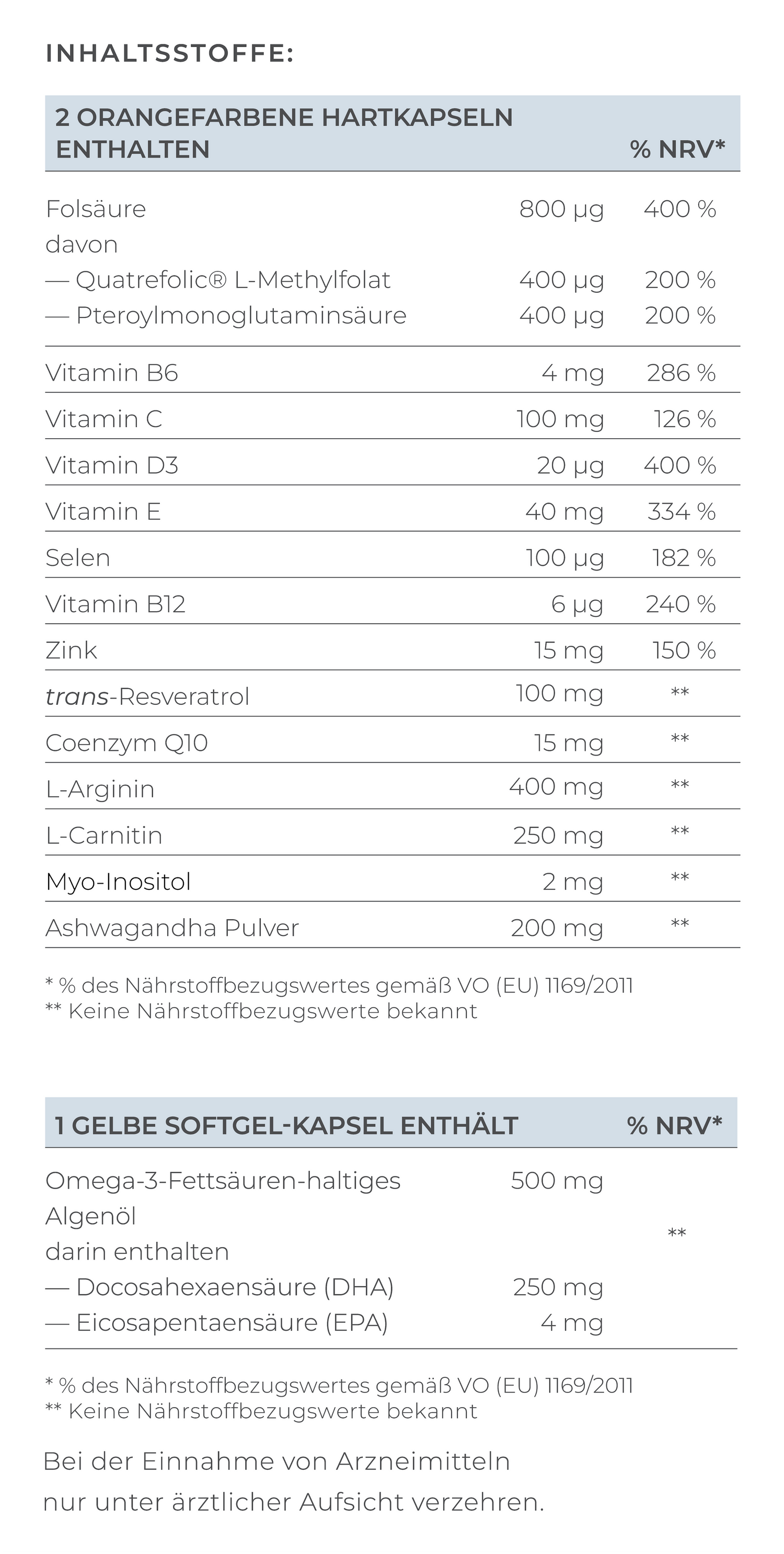
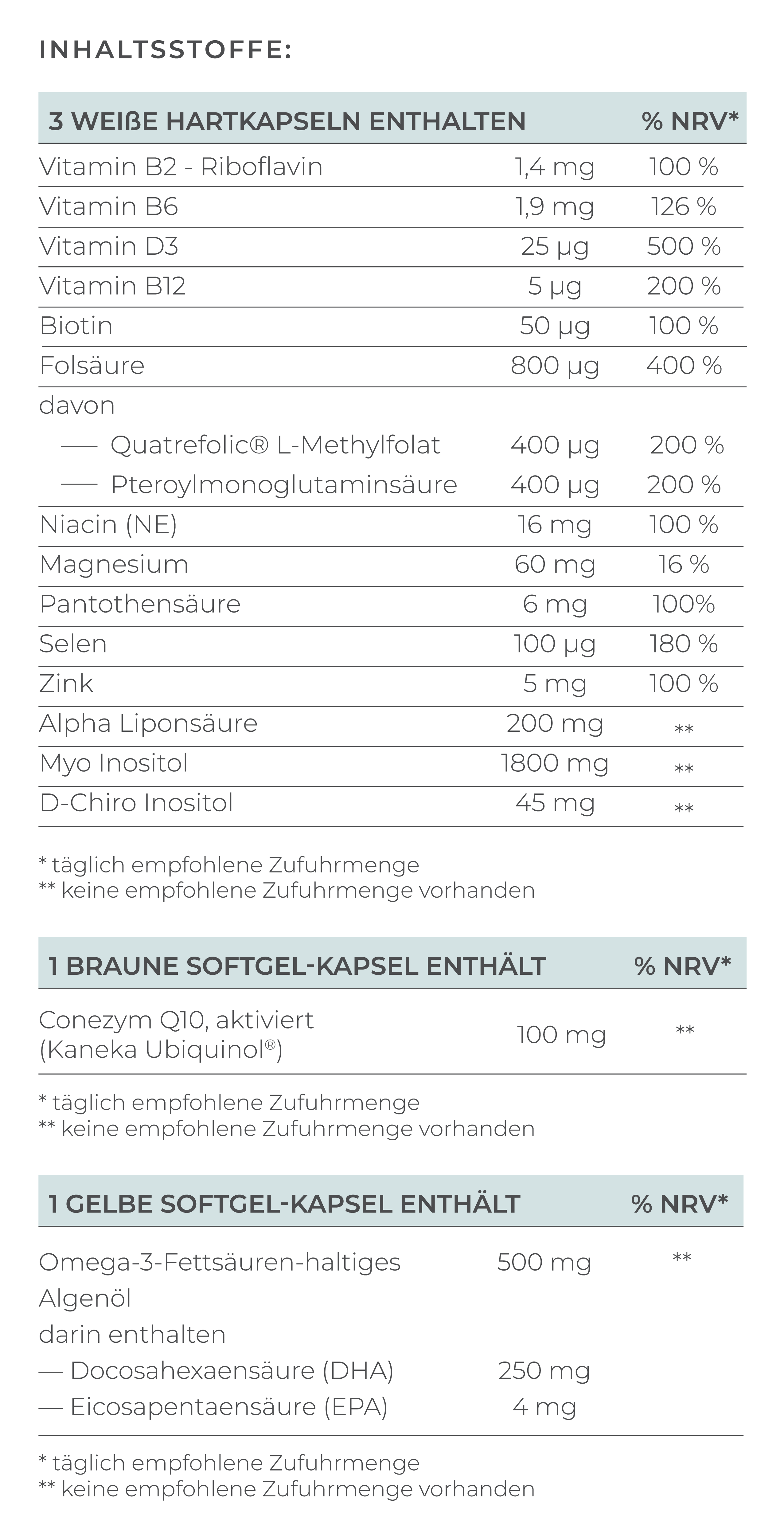
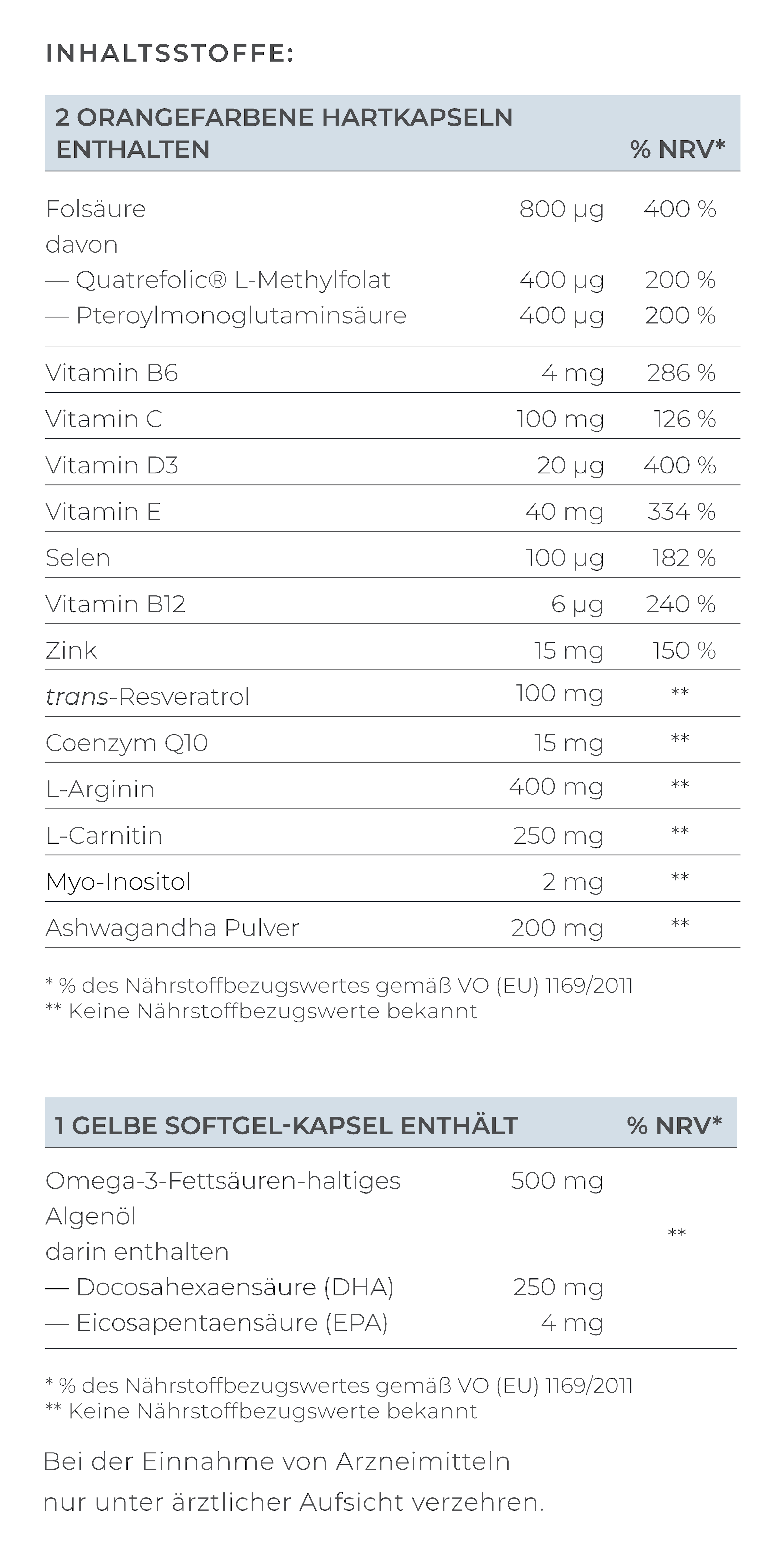
- Folic acid: Essential for cell division and healthy embryo development. Approx. 400-800 µg daily is recommended, even before the start of treatment.
- Omega-3 fatty acids (e.g. from fish oil, linseed oil): Have an anti-inflammatory effect and support implantation.
- Antioxidants (vitamins C, E, coenzyme Q10, zinc, selenium): Protect cells from oxidative stress, which can damage eggs and sperm.
- Iron and vitamin D: Support hormone balance and the endometrium.
- Complex carbohydrates and fiber: Keep blood sugar stable, which promotes hormonal balance.
Nutrition tips before and during IVF
- Avoid highly processed foods, sugar and trans fats.
- Eat plenty of fresh fruit and vegetables, whole grain products and healthy fats.
- Make sure you get enough protein (preferably plant-based and low-fat animal sources)
- Drink enough water - good hydration supports circulation and metabolism.
- Avoid alcohol, nicotine and drugs as these can affect fertility.
How else can I prepare for IVF?
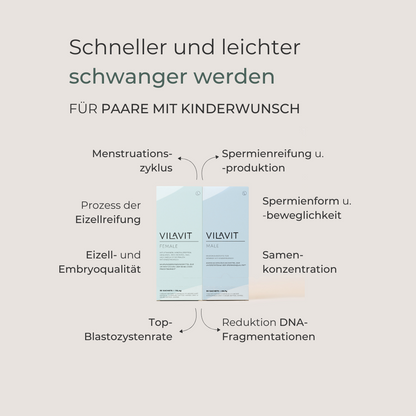
- Micronutrient supplements: Many women take specially formulated supplements to support egg quality (“Pimp my Eggs”) and men take special products to improve sperm quality (“Pimp my Sperm”). Such supplements often contain a combination of the nutrients mentioned. Consultation with your doctor is always recommended.
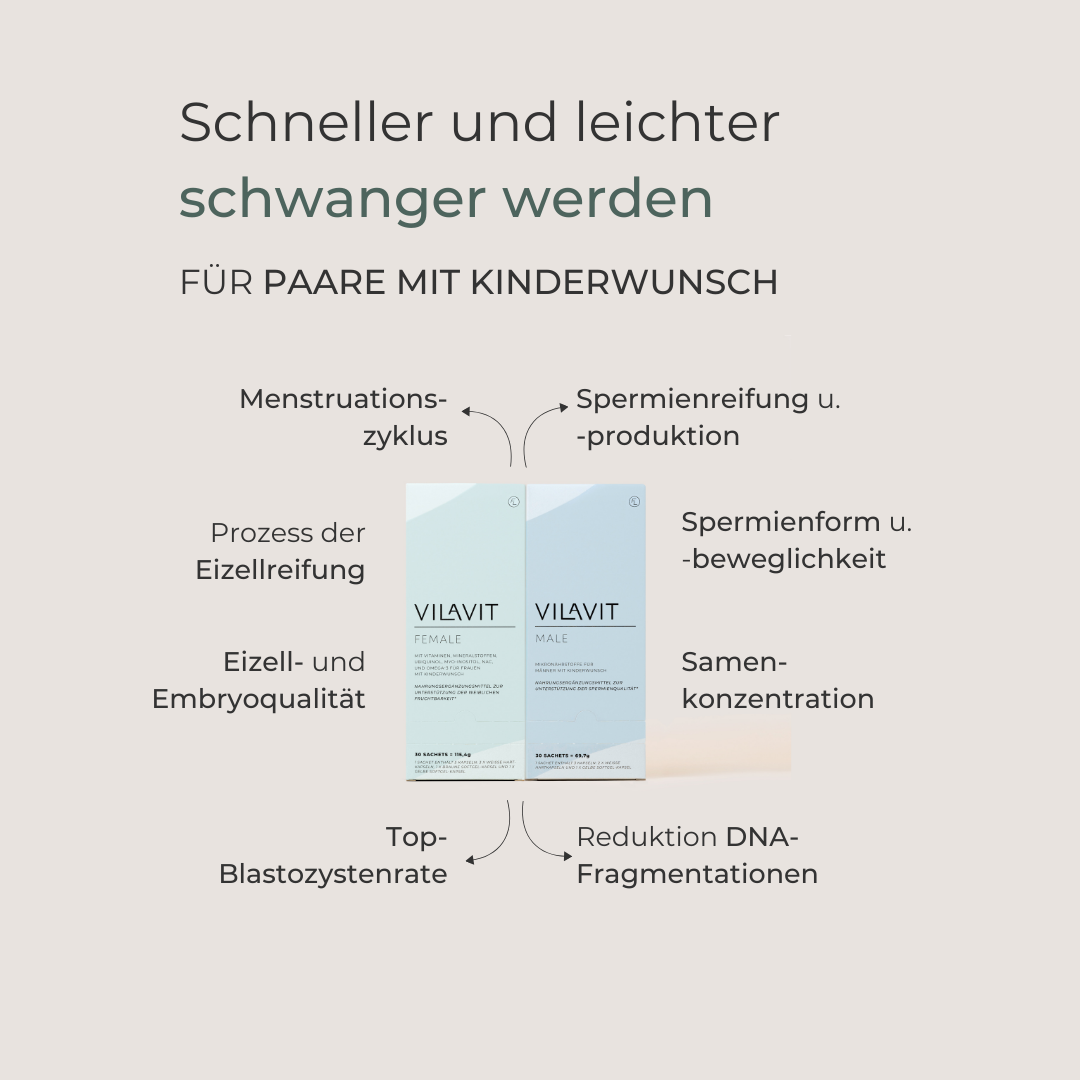
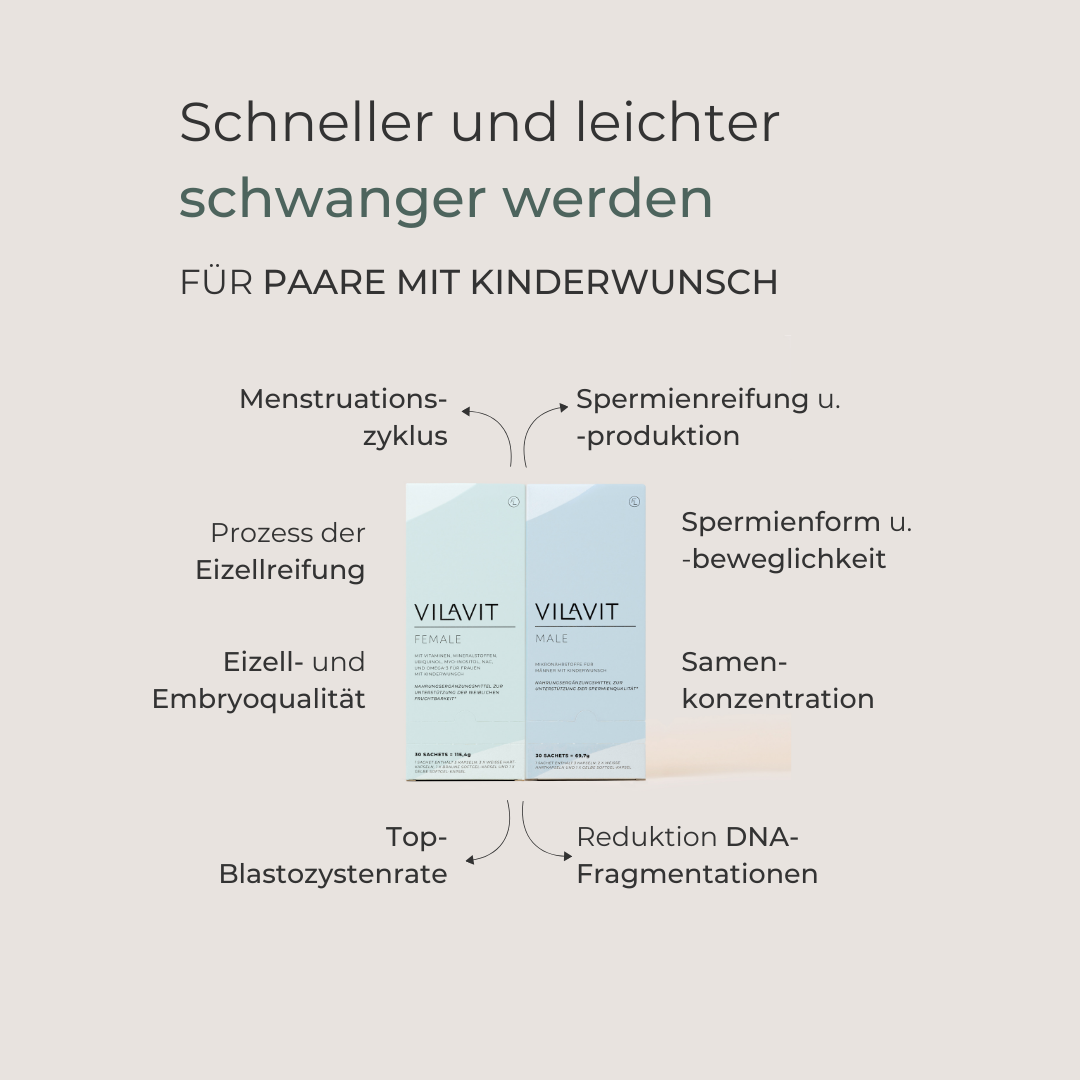
With VILAVIT Female and VILAVIT Male, you have a practical solution at hand: both products provide all the essential micronutrients to support your fertility and increase your chances of successful IVF.
- Stress reduction: Stress has a negative effect on hormone levels and fertility. Relaxation techniques such as yoga, meditation or autogenic training can help you to cope better with the treatment process.
- Exercise: Moderate, regular physical activity - such as walking, swimming or yoga - promotes blood circulation and makes you feel better. However, overly intensive training should be avoided. Regular exercise helps to reduce stress, balance hormone levels and releases endorphins, which help to cope better with the stressful situation of IVF.
- Sufficient sleep: A healthy sleep rhythm is important for the woman's hormone balance and for the man's sperm maturation.
- Weight: A healthy body weight (BMI in the normal range) improves fertility and the success of treatment. Both being underweight and overweight can cause hormonal imbalances.
- Stay informed: If you are familiar with the process and the various treatment options, you can have a better say and feel more confident about the decisions you make during treatment.
FAQ about the IVF process
Which is better, IVF or ICSI?
IVF (in vitro fertilization) and ICSI (intracytoplasmic sperm injection) are both assisted fertilization methods. Which method is better depends on the individual causes of infertility:
- IVF is well suited if the sperm quality is still sufficient and natural fertilization in a test tube appears possible.
- ICSI is used if the sperm quality is severely limited (e.g. very few or non-motile sperm) or in the case of previous IVF failures. A single sperm is injected directly into the egg, which can increase the chances of fertilization.
The choice of procedure is made by the treating doctor on an individual basis, depending on the medical history and diagnosis.
How long does an IVF process take?
The entire IVF process usually takes around 4 to 6 weeks per cycle, divided into different phases:
- Preparation and initial examinations (1 week)
- Hormonal stimulation of the ovaries (8 to 14 days)
- Egg retrieval (follicular puncture) and fertilization in the laboratory (1 day)
- Embryo cultivation (2 to 5 days)
- Embryo transfer and subsequent resting phase until pregnancy test (approx. 2 weeks)
The exact duration may vary depending on individual requirements and treatment plan.
What is IVF naturelle?
IVF naturelle (natural IVF) is a variant of in vitro fertilization in which no or very little hormonal stimulation is used. Only the egg cell that matures in the natural cycle is used, without additional medication for follicle maturation. This results in a gentler process with fewer side effects, but the chances of several eggs being retrieved and therefore pregnancy are lower than with conventional IVF with stimulation. Natural IVF is particularly suitable for patients who prefer drug-free treatment or who respond poorly to hormonal stimulation.