Everything you need to know about chronic endometritis when trying to conceive
-
Chronic endometritis often progresses without any noticeable symptoms - so it remains undetected for a long time.
-
The inflammation can prevent the embryo from implanting in the lining of the uterus.
-
Certain immune cells are elevated in many of those affected and interfere with the healthy development of the child.
-
Studies show that more than half of women with unexplained infertility could be affected.
-
Targeted antibiotic therapy can successfully eliminate the inflammation in over 90% of patients.
Uterine inflammation is a common cause of miscarriages
Chronic endometritis is a condition that is often asymptomatic and goes unnoticed, but can have a significant impact on fertility. Especially in women with repeated implantation failure or repeated miscarriages, the disease is considered to be of increasing importance (Lucan, 2025).
What is chronic endometritis?
Endometritis is an inflammation of the lining of the uterus, the endometrium. If this inflammation persists over a longer period of time, it is referred to as chronic endometritis. This condition is often asymptomatic, which means that those affected may not notice any obvious signs.
How common is chronic endometritis?
A comprehensive meta-analysis of 2024 showed that chronic endometritis was significantly more common in infertile women than in the control group (19.46% vs. 7.7%). Particularly noteworthy is the high prevalence in women with recurrent miscarriages (37.6% vs. 16.4% in the control group) (Ticconi, 2024).
A study of women who were examined for infertility showed that significantly more than half suffered from chronic endometritis - although they had no clear cause for their infertility beforehand (idiopathic infertility). This suggests that this undetected inflammation occurs more frequently than previously assumed and could play an important role in unexplained infertility (Gu et al., 2023).
Can you get pregnant with inflammation in the uterus?
Yes, you can have children with chronic endometritis. However, chronic inflammation of the uterine lining can significantly reduce the chances of pregnancy. However, treating chronic endometritis with antibiotics can significantly increase the chances of a successful pregnancy and thus help make your path to your dream child easier.
What are the symptoms of chronic endometritis?
- Irregular or prolonged menstrual bleeding
Spotting, intermenstrual bleeding or excessively heavy periods
- Chronic lower abdominal or pelvic pain
Often diffuse pain that can last for months
- Vaginal discharge (usually yellowish, foul-smelling)
May indicate an accompanying bacterial infection
- Pain during sexual intercourse (dyspareunia)
Often associated with inflammatory changes to the uterine lining
- Subfertility or unfulfilled desire to have children
- Asymptomatic course
In many cases, chronic endometritis goes unnoticed and is only diagnosed following a uterine biopsy
How can chronic endometritis be diagnosed?
The diagnosis is usually made through a biopsy of the uterine lining (endometrial biopsy), in which a small sample of the uterine lining is taken. This biopsy can be carried out as part of a gynecological examination or by means of a hysteroscopy (endoscopy of the uterine cavity) (Gu, 2023).
Depending on how much pain is felt, the procedure can be performed under local anesthesia, with painkillers or without any medication at all.
Histological and immunohistochemical examination
Ideally, immunohistochemical staining of the biopsy material is used for histological examination, in particular with the marker CD138 (Syndecan-1).
This is used for the targeted visualization of plasma cells, which are a central histological feature of chronic endometritis (Herlihy, 2022).
Molecular diagnostics
In addition to histological assessment, molecular diagnostics can also be carried out in specialized laboratories. This includes
-
PCR-based detection (e.g. 16S rRNA gene sequencing) to identify bacterial DNA, particularly of chronically persistent pathogens such as Gardnerella vaginalis, Enterococcus faecalis, Escherichia coli or Mycoplasma/Ureaplasma.
-
Use of so-called microbial panels to visualize the uterine microbiome and potential dysbioses.
These molecular diagnostic procedures can help to detect low-grade or atypical infections that cannot be clearly identified histologically - particularly in patients with an unfulfilled desire to have children or repeated implantation failures following artificial insemination.
Note: Molecular diagnostics are not part of standard diagnostics and are primarily used in reproductive medicine centers.
What are the causes of chronic endometritis?
The exact causes of chronic endometritis are not always clear, but there are some factors that may increase the risk, including:
-
Bacterial infections: Chronic infections in the genital tract, particularly from bacteria such as chlamydia or gonorrhea, can lead to inflammation of the endometrium.
-
Instrumental interventions: Previous uterine interventions such as caesarean section, scraping or hysteroscopy can increase the risk of chronic endometritis.
-
Hormonal disorders: Imbalances in hormone levels, particularly a lack of progesterone, can promote the development of chronic endometritis.
-
Weakening of the cervix: A weakened cervix, for example after a previous birth or the insertion of an IUD, can make it easier for infections to develop due to germs that can occur in hospital, for example.
What treatment options are there?
The treatment of chronic endometritis is usually aimed at eliminating the underlying inflammation and regenerating the endometrium.
The classic therapy is antibiotic therapy: taking antibiotics can effectively combat the inflammation. The standard therapy consists of doxycycline 100mg twice a day for 14 days (Odendaal, 2023).
Studies confirm that effective treatment of chronic endometritis significantly increases the chances of a successful pregnancy. Women who have suffered repeated miscarriages also benefit from successful treatment, as the chance of a live birth increases significantly thanks to antibiotic therapy (Holzer, 2023).
Targeted treatment can also improve the chances of success of further in vitro fertilization treatments in cases of repeated implantation failure after artificial insemination (Vitagliano, 2018). In these cases, it may be useful to check whether the inflammation has actually healed completely before a new IVF cycle or whether further antibiotic therapy is advisable before another IVF attempt.
Despite the high effectiveness of this therapy (over 90% cure), there are differing opinions as to whether a second biopsy is necessary to confirm cure (AWMF, 2022).
What effects does chronic endometritis have on the desire to have children?
Chronic endometritis can have a significant impact on fertility:
Impairment of implantation
Studies show that women with chronic endometritis often have different ratios of certain cells that are important for the function of the immune system. It can therefore be concluded that these cells not only impair implantation, but can also have a negative impact on the further course of the pregnancy. However, after successful antibiotic therapy, these values and ratios usually normalize and the chance of a successful pregnancy increases (Li et al., 2020).
Changes to the lining of the uterus
Chronic inflammation of the lining of the uterus (chronic endometritis) causes the tissue to change in various ways:
-
Scarring (fibrosis) and shrinkage of the mucosal glands, which causes the “soft, nourishing” tissue to recede.
-
Malformation of the blood vessels, so that the mucous membrane is less well supplied with blood.
-
Alteration of important body signals that normally enable the embryo to grow.
These changes make it harder for the uterine lining to accommodate and nourish an embryo - which is considered the main cause of implantation problems and early pregnancies (Lucan, 2025).
Increased miscarriage rate
Women with chronic endometritis have an increased risk of habitual miscarriages. Studies show that bacteria or chronic inflammation often damage the endometrium in affected women, making it more difficult for an embryo to implant or develop. Clinical studies show that targeted antibiotic therapy significantly increases the pregnancy rate in affected women - from less than 20% before therapy to over 75% after successful therapy (Pirtea, 2021).
What can those affected do?
-
If you are unable to conceive, consult a specialist gynaecologist or fertility clinic and ask specifically about chronic endometritis.
-
Maintain a healthy lifestyle: balanced diet, exercise, stress reduction.
-
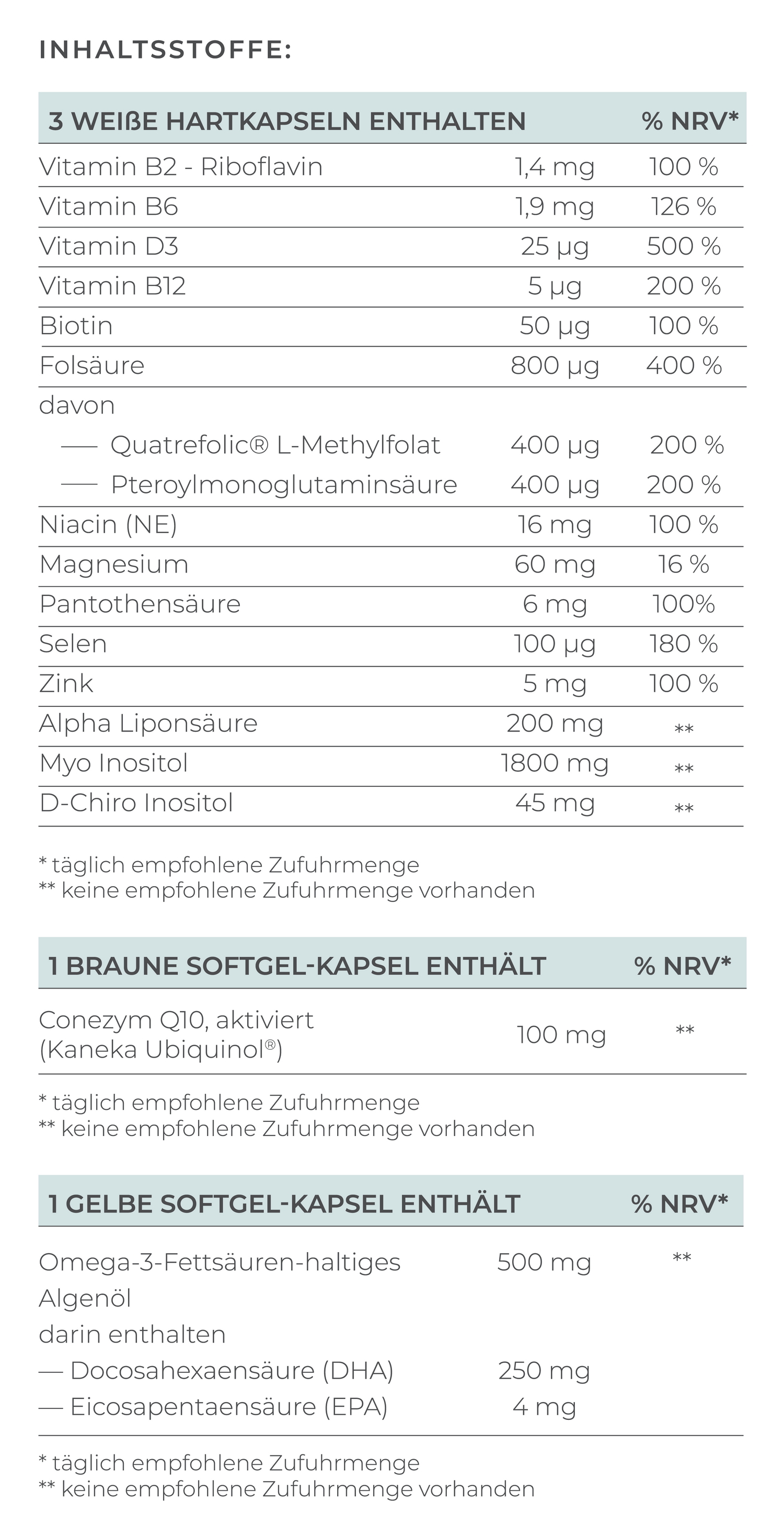
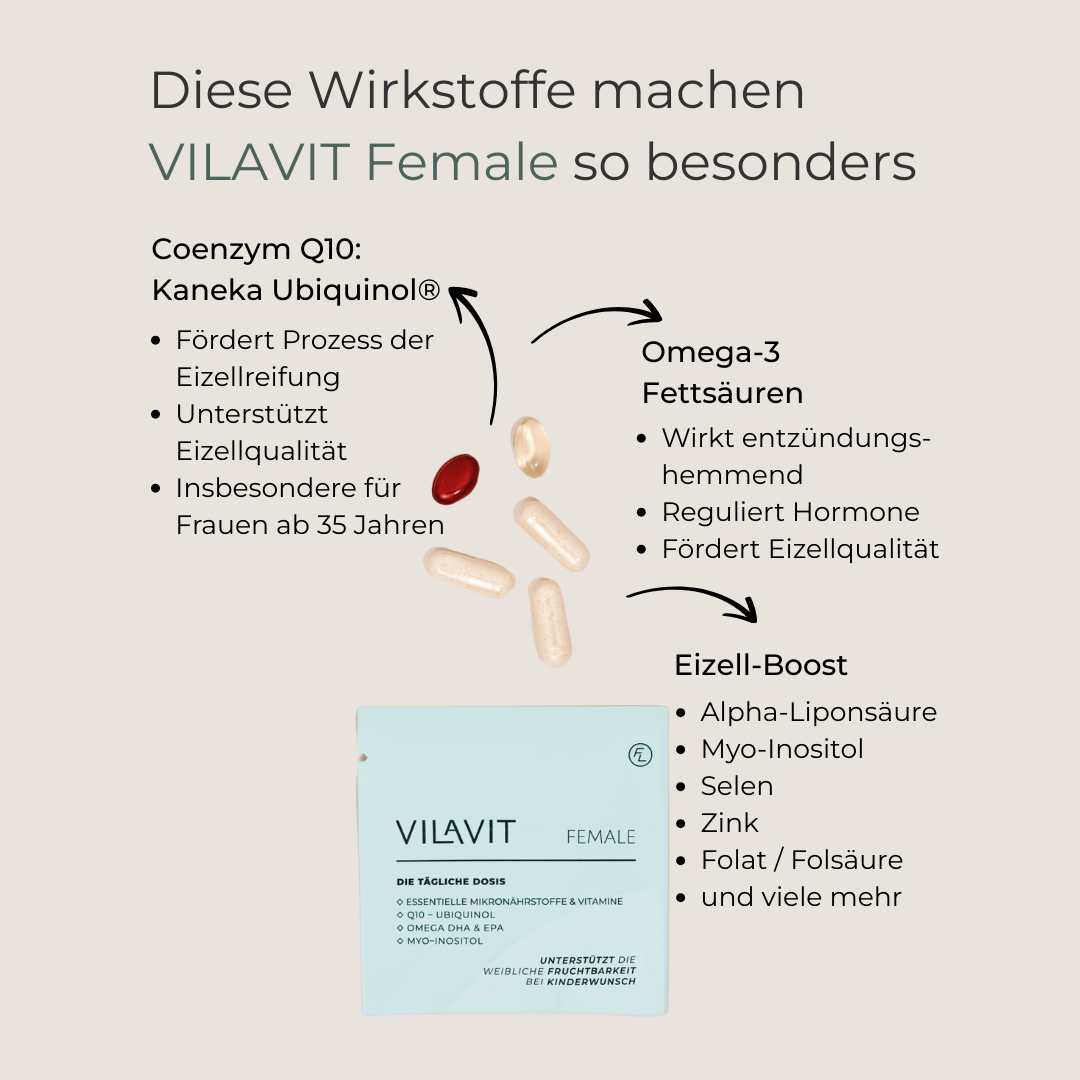
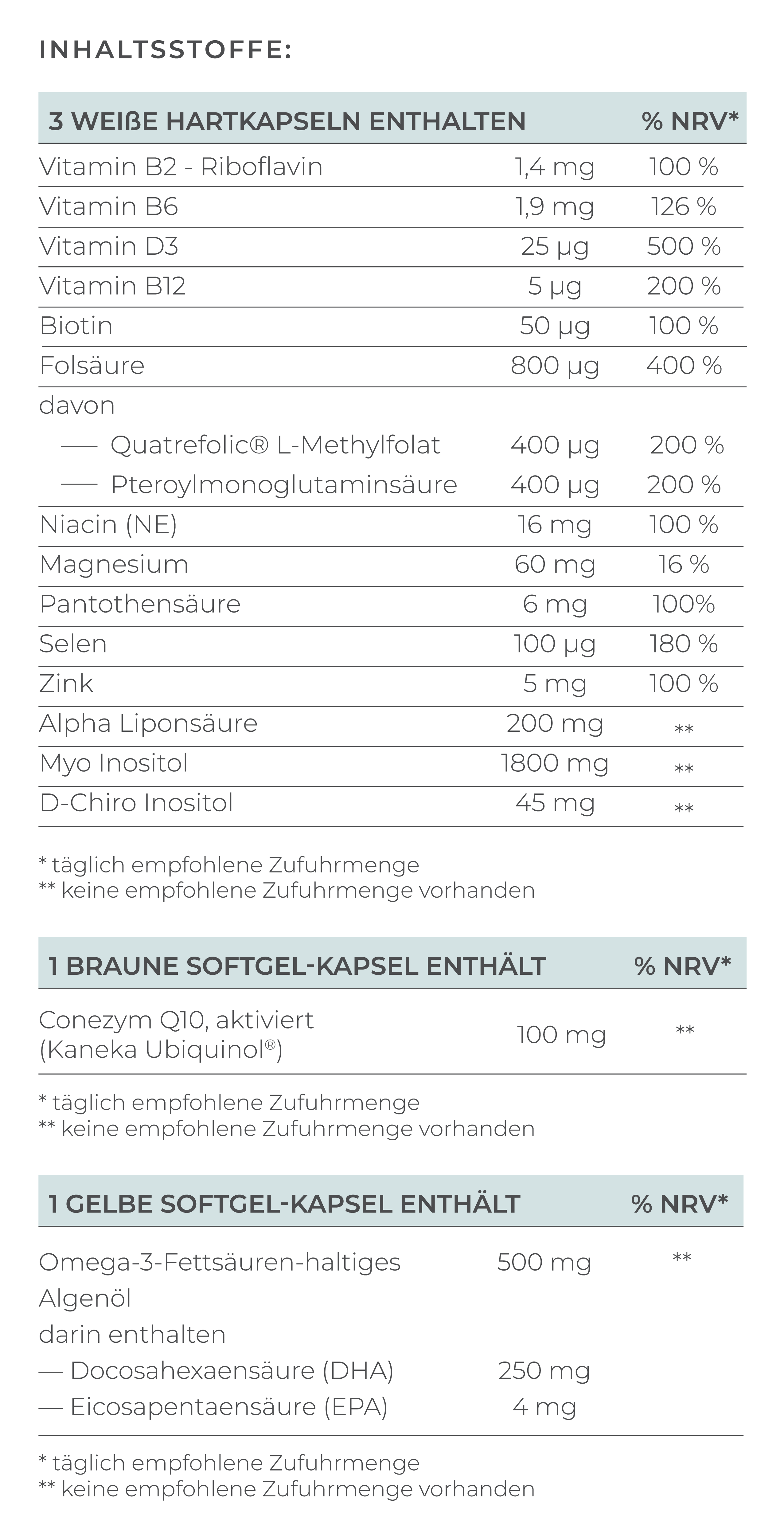
Micronutrients can support fertility - VILAVIT Female, for example, can help to provide the body with an optimal supply of important vitamins and minerals.
Conclusion & tip
Chronic endometritis is an often overlooked but easily treatable cause of infertility. Anyone affected should not be discouraged and should specifically ask for clarification. Successful treatment can significantly increase the chances of pregnancy.
And: with a targeted supply of high-quality and bioavailable micronutrients, the body can be given additional support to make the dream of having a child a reality.
FAQ: Frequently asked questions about chronic endometritis when trying to conceive
Can chronic endometritis affect fertility even without symptoms?
Yes. Even if there are no symptoms, the inflammation can interfere with implantation or prevent pregnancy. A biopsy provides clarity.
What is the difference between chronic and acute endometritis?
The acute form usually occurs suddenly after infections or interventions. Chronic endometritis often progresses gradually and causes long-term changes to the mucous membrane.
Is pregnancy possible despite chronic endometritis?
In principle, yes - but the probability is reduced. After targeted treatment, the chances increase significantly.
When should I consider a biopsy?
An endometrial biopsy is particularly useful in the case of an unexplained desire to have children, repeated miscarriages or implantation failure - even without symptoms.
How long does the treatment of chronic endometritis take?
Antibiotic therapy usually lasts two weeks. Some centers recommend a follow-up biopsy to ensure the success of the treatment.