-
Female infertility affects many women, yet the topic often remains hidden.
-
The most common causes include reduced egg quality, PCOS, ovulation disorders, and endometriosis.
-
Diagnosis of female infertility usually begins with a medical consultation, hormone analysis, and an ultrasound examination.
-
The path to parenthood can range from cycle monitoring to fertility treatments.
-
An active, healthy lifestyle and targeted micronutrients are important building blocks to optimally support egg quality.
The key points in brief
-
Definition
Female infertility occurs when a woman is unable to conceive despite having regular, unprotected intercourse for one year.
-
Symptoms
Symptoms can vary and are often nonspecific. They may include irregular menstrual cycles, pelvic pain, unusual bleeding, or hormonal imbalances.
-
Causes of Female Infertility
Common causes of female infertility include ovulation problems, anatomical abnormalities of the reproductive organs, endometriosis, hormonal disorders such as PCOS (polycystic ovary syndrome), infections, age, and lifestyle factors like smoking and excessive alcohol consumption.
-
Treatment of Infertility
Treatment options include micronutrient supplementation, hormone therapy to stimulate ovulation, intrauterine insemination (IUI), in vitro fertilization (IVF), possible surgical correction of anatomical issues, and lifestyle-oriented measures such as weight management and smoking cessation.
-
Diagnosis
The diagnosis includes a detailed medical consultation, a gynecological examination including ultrasound, assessment of hormone levels, and, if necessary, specific tests such as hysterosalpingography to check the patency of the fallopian tubes.

Female Infertility
Many women face unexpected challenges on their journey to having a child. Female infertility is a common issue that quietly affects many couples and is often accompanied by uncertainty and questions. According to the World Health Organization (WHO), infertility is defined as the inability of a woman to conceive after one year of regular, unprotected intercourse during her fertile days.
Causes of Female Infertility
Endometriosis
Endometriosis occurs when the uterine lining (endometrium) grows outside the uterus. This can lead to inflammation and reduced fertility. About 5 to 10% of all women suffer from endometriosis. Fertility is not only impaired, but the risk of complications during pregnancy and miscarriage is also increased.
In many women, the detached tissue, called endometriotic lesions, can shed unnoticed and without pain. In others, these tissue remnants cause inflammation, cysts, and adhesions, leading to varying degrees of menstrual pain as well as pain in the affected areas. The pain is often cramp-like and may be accompanied by nausea, vomiting, or diarrhea.
Polycystic Ovary Syndrome (PCOS)
Polycystic Ovary Syndrome (PCOS) is one of the most common hormonal disorders affecting women of reproductive age. In Europe, 5 to 10% of women are affected, often without realizing it. Although the name suggests "many cysts", PCOS actually involves numerous follicles that do not mature properly due to hormonal imbalances.
Women with PCOS often have low levels of FSH (follicle-stimulating hormone) and high levels of LH (luteinizing hormone). Due to the FSH deficiency, the follicles fail to mature. Ovulation does not occur, and no progesterone (corpus luteum hormone) is produced. Menstrual cycles in affected women are usually very long, with infrequent or absent bleeding. Additionally, 75% of women with PCOS have increased insulin resistance.
The elevated insulin levels, necessary for glucose uptake, stimulate androgen production in the ovaries, leading to higher concentrations of male hormones (androgens).
Symptoms:
PCOS is characterized by irregular or absent menstrual periods. Ovulation often does not occur. Triggers can include mild overweight and elevated androgen levels. Other symptoms include acne and increased body hair growth.
Blocked Fallopian Tubes
The fallopian tubes connect the ovaries to the uterus. They are crucial for fertilization because the egg travels through the fallopian tube, where it is fertilized by the sperm in the ampulla of the tube. However, fallopian tubes can become blocked, scarred, or stuck together due to inflammation and infections (commonly chlamydia or gonorrhea) or due to endometriosis.
Hormonal Disorders
Hormonal disorders are usually recognizable by changes in the menstrual cycle. Bleeding may be absent, irregular, or there may be spotting and breakthrough bleeding. Thyroid dysfunctions are often a cause of infertility. Thyroid hormones influence the cycle, female fertility, and the brain development of the unborn child.
Hypothyroidism
Cause: often Hashimoto's thyroiditis
Symptoms: fatigue, dry eyes, hoarseness, constipation, or weight gain
Impact on female fertility: cycle disorders, prolonged cycle, rare bleeding or ovulation, miscarriages
Hyperthyroidism
Cause: often Graves' disease
Symptoms: high blood pressure, heart arrhythmias, nervousness, weight loss, diarrhea, excessive sweating, sleep disorders, hair loss, exhaustion, mood swings
Impact on female fertility: cycle disorders
Hyperprolactinemia (increased prolactin levels)
Cause: often hypothyroidism, medications (antidepressants), stress
Impact on female fertility: cycle disorders, no or rare egg maturation
Hyperandrogenemia (increased male hormones)
Possible causes: PCOS, androgenital syndrome (metabolic disorder), ovarian tumor
Impact on female fertility: lack of egg maturation and absent ovulation
Luteal phase defect (progesterone deficiency)
Symptoms: spotting in the second half of the cycle, too short luteal phase, sleep disturbances
Impact on female fertility: problems with embryo implantation. The luteal hormone (progesterone) is responsible for the implantation of the fertilized egg.
Myomas & Polyps
Myomas are common benign lumps in the uterus. Nodules in the uterine cavity or wall can make embryo implantation more difficult. Depending on their size, they can be removed through minimally invasive surgery.
Polyps are benign and usually harmless growths of the uterine lining. They often shed during the next menstrual period. However, a poorly positioned polyp can affect fertility. Polyps can be removed by curettage.
Symptoms: Myomas or polyps are often unnoticed.
Uterine malformations
The uterus is an inverted pear-shaped muscular organ, a smooth cavity lined with mucosa where an embryo can develop. Any malformation of the uterus can affect fertility. There are different types of malformations:
Uterus arcuatus: The heart-shaped uterus is the mildest form of malformation. Here, the upper part of the uterus has a small indentation, giving it a heart-like shape. It appears to have no impact on female fertility or implantation.
Uterus septus: A partition of varying length and thickness is present inside the uterus. This can restrict fertility and increase the risk of miscarriage.
Malformations can be treated surgically, making natural pregnancy possible.
Premature menopause
Premature menopause is the permanent end of the menstrual period before the age of 40. It occurs when the ovaries no longer regularly release eggs and ovulation stops. Premature menopause is accompanied by a hormonal adjustment in the female body.
Symptoms: While some women experience no symptoms, others suffer from common menopausal symptoms such as hot flashes, mood swings, and night sweats.
Possible causes: Genetic abnormalities, autoimmune diseases, viral infections, surgical removal of the ovaries and uterus, chemotherapy or radiation therapy, and toxins such as tobacco.
Immune system disorders
The cause of female infertility can also lie in a disrupted immune response of the female body. The immune system mistakenly identifies the embryo as a foreign body and attacks it as an intruder.
Diagnosis of Female Infertility
The diagnosis of the cause of infertility is crucial to choose the appropriate treatment.
Ultrasound examination
An ultrasound examination allows important functions of the uterus to be assessed. The structure, position, and size of the uterus, as well as possible conditions such as fibroids, polyps, or ovarian cysts, can be diagnosed. Ultrasound is also relevant for monitoring the maturation of follicles and the uterine lining, as well as for tracking the absence of the menstrual cycle.
Tubal examination using HyCoSy
Using ultrasound technology (hysterosalpingo-contrast sonography, "HyCoSy"), the patency of the fallopian tubes can be examined largely painlessly. During a HyCoSy, an echogenic foam is gently introduced into the uterine cavity through a thin catheter. This allows both fallopian tubes to be checked for openness and monitored in real time via ultrasound. The advantages of HyCoSy include significantly lower radiation exposure compared to the previously common tubal X-ray examination (hysterosalpingography, HSG). Unlike operative laparoscopy, the tubal examination with HyCoSy is non-invasive.
Endometrial biopsy
An examination of the endometrium can provide insights into natural "killer cells" (NK cells) and plasma cells. During an endometrial biopsy, small tissue samples of the uterine lining are taken using a catheter and then analyzed microscopically.
Gynecological examination
During a gynecological examination, initial signs of endometriosis, fibroids, and ovarian cysts can already be detected.
Medical history
It is important to review the personal medical history, including cycle regularity, any previous gynecological conditions, surgeries, and medications.
Hormone status
Since hormonal disorders are often a cause of infertility, it is advisable to test hormone levels. The hormone profile and its fluctuations during the cycle provide important insights into female fertility. The ovarian reserve is also assessed based on hormone values. Between the second and fifth day of the cycle, the following levels are crucial: FSH, LH, TSH, estrogens, prolactin, and androgens. In the second half of the cycle, progesterone and estrogen levels can be particularly informative.
Laparoscopy
If adhesions, scar tissue, or endometriosis are suspected, diagnosis can be performed using laparoscopy. Under anesthesia, a laparoscope, a tube-shaped instrument, is inserted into the abdominal cavity through a small incision in the abdomen. This instrument provides a detailed view of the internal reproductive organs, which can be displayed on an external monitor.
Hysteroscopy
If malformations of the uterus or changes in the uterine lining are suspected, further diagnostics as well as simultaneous treatment can be performed using hysteroscopy.
The way to parenthood
The underlying cause of infertility largely determines the choice of appropriate therapy. Common treatment options include cycle monitoring, hormonal stimulation, insemination, in vitro fertilization (IVF), and intracytoplasmic sperm injection (ICSI).
Since the fertile days are close to ovulation, it is crucial to know them. Cycle monitoring can be done independently if the cycle is regular, but fertility centers often provide support through ultrasound and hormone diagnostics. This allows monitoring of the follicle's maturation and prediction of ovulation. Sexual intercourse is recommended shortly before ovulation. Pregnancy can thus occur naturally using this method.
Hormonal stimulation is an important step in fertility treatment, especially when ovulation does not occur. First, the female cycle is closely monitored to identify hormonal causes such as polycystic ovary syndrome (PCOS), thyroid disorders, or elevated prolactin levels. Through targeted hormone therapies, the ovaries can be stimulated and the cycle normalized, making natural pregnancy at home possible again.
Intrauterine insemination (IUI) is a fertility treatment in which specially prepared sperm are directly placed into the uterus around the time of ovulation. This procedure increases the chances of sperm reaching the egg and can be combined with ovarian stimulation to improve the likelihood of conception. IUI is often recommended for couples with mild male infertility, unexplained infertility, or cervical mucus problems.
In in-vitro fertilization (IVF), fertilization takes place outside the body in a laboratory dish. Eggs are combined with sperm in a petri dish to facilitate fertilization. ICSI (intracytoplasmic sperm injection) is a specialized form of IVF in which the best sperm is selected under a microscope and carefully injected directly into the egg. The ICSI method is necessary when sperm quality is severely impaired.

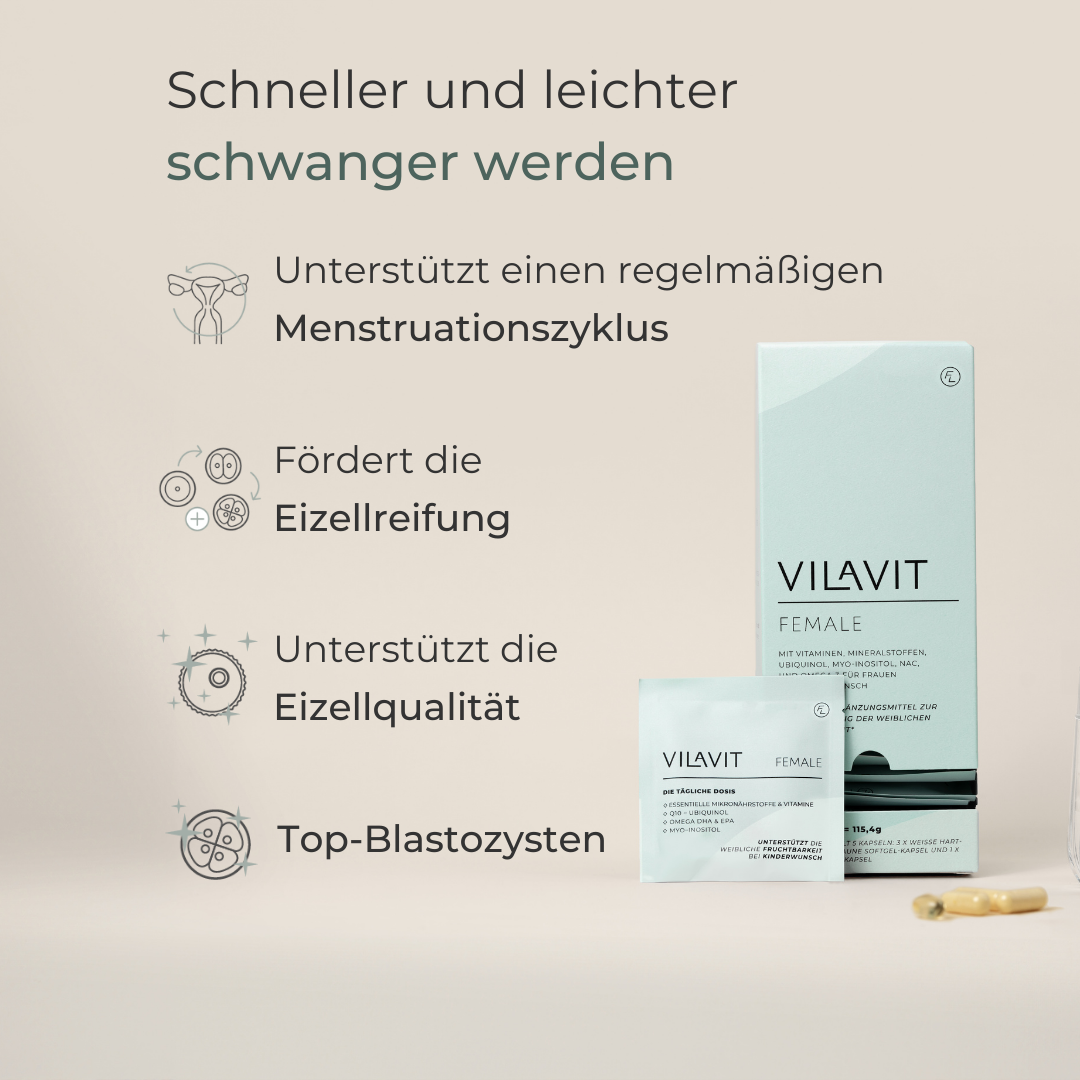
Pimp you Eggs: Boost your fertility
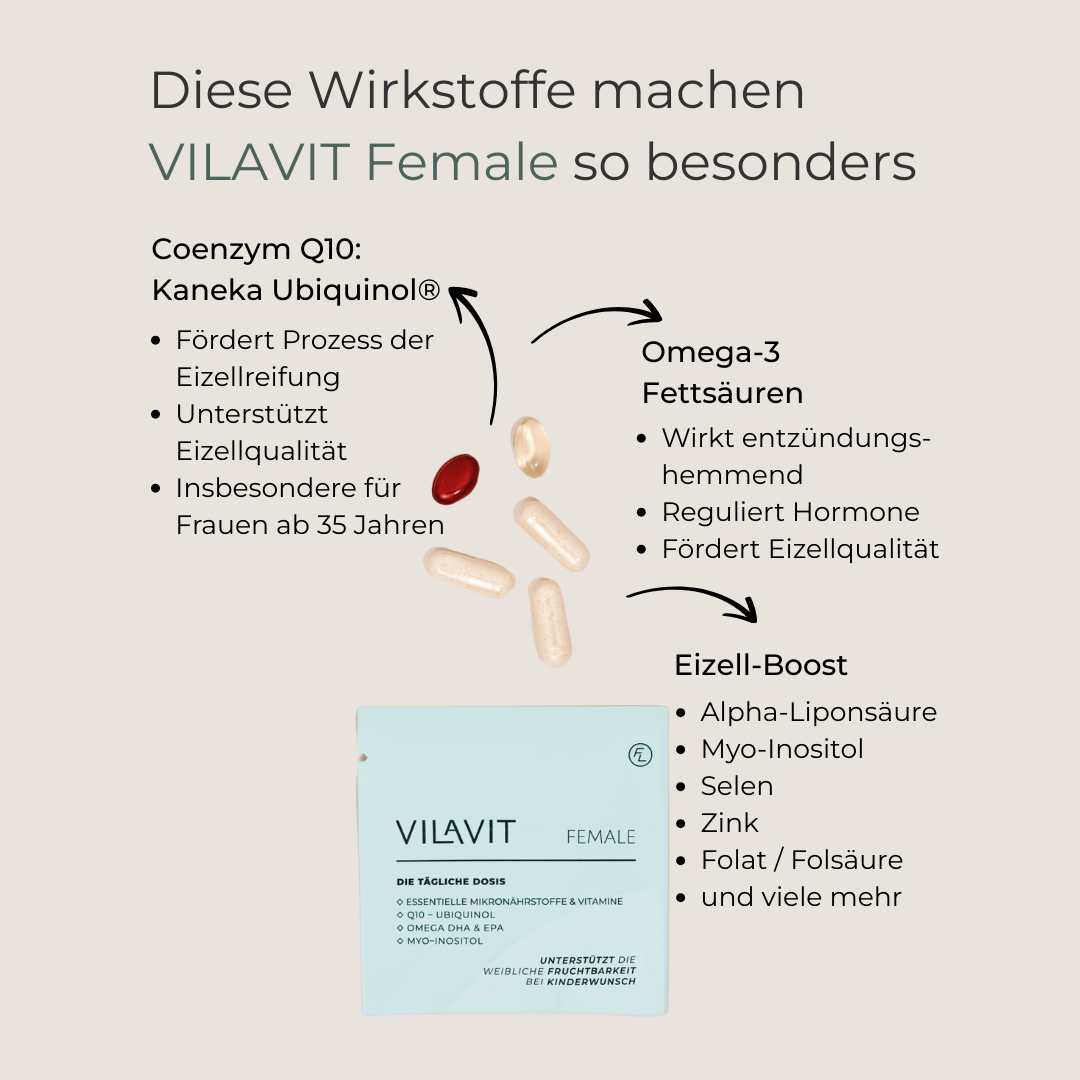
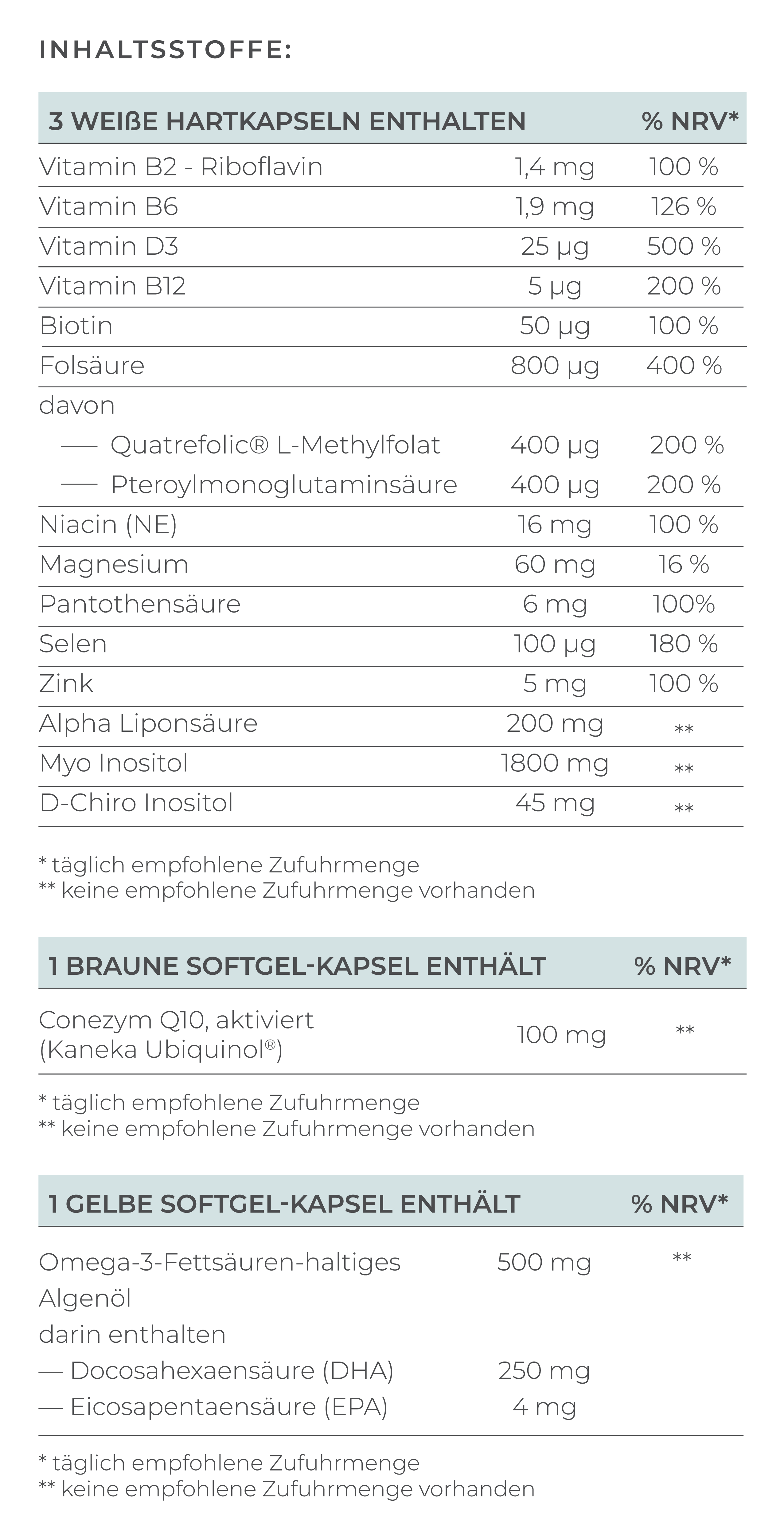
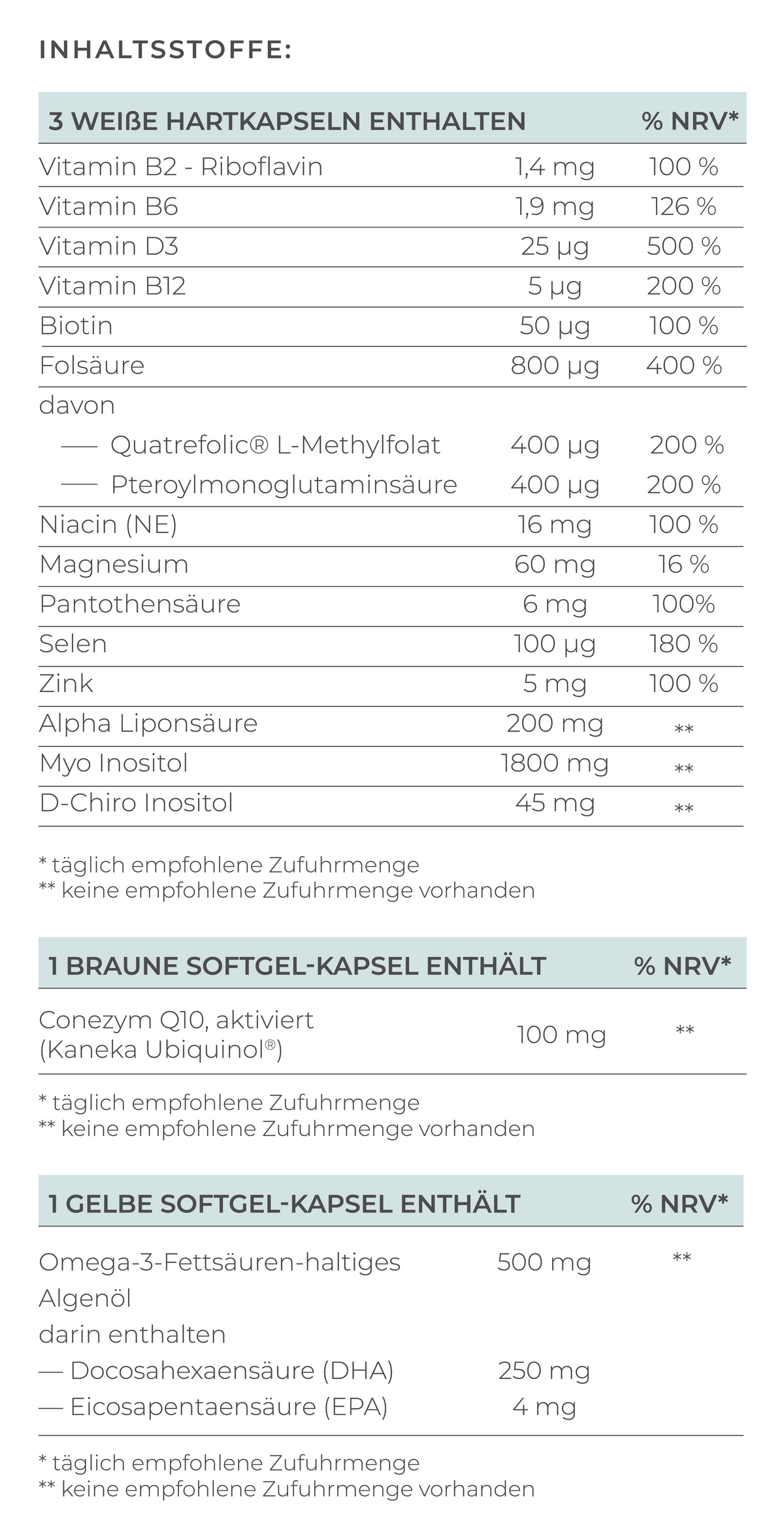
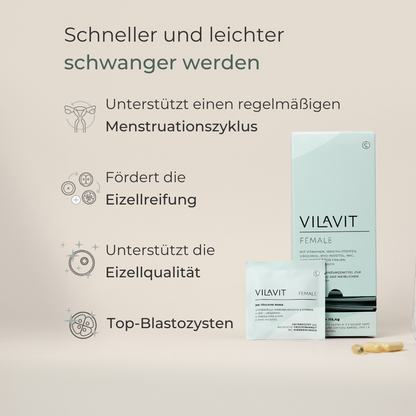
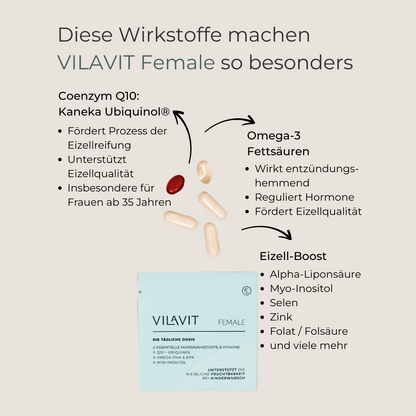
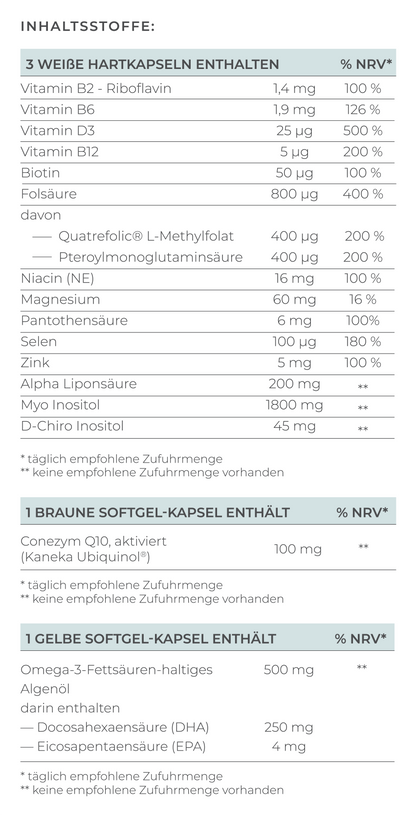
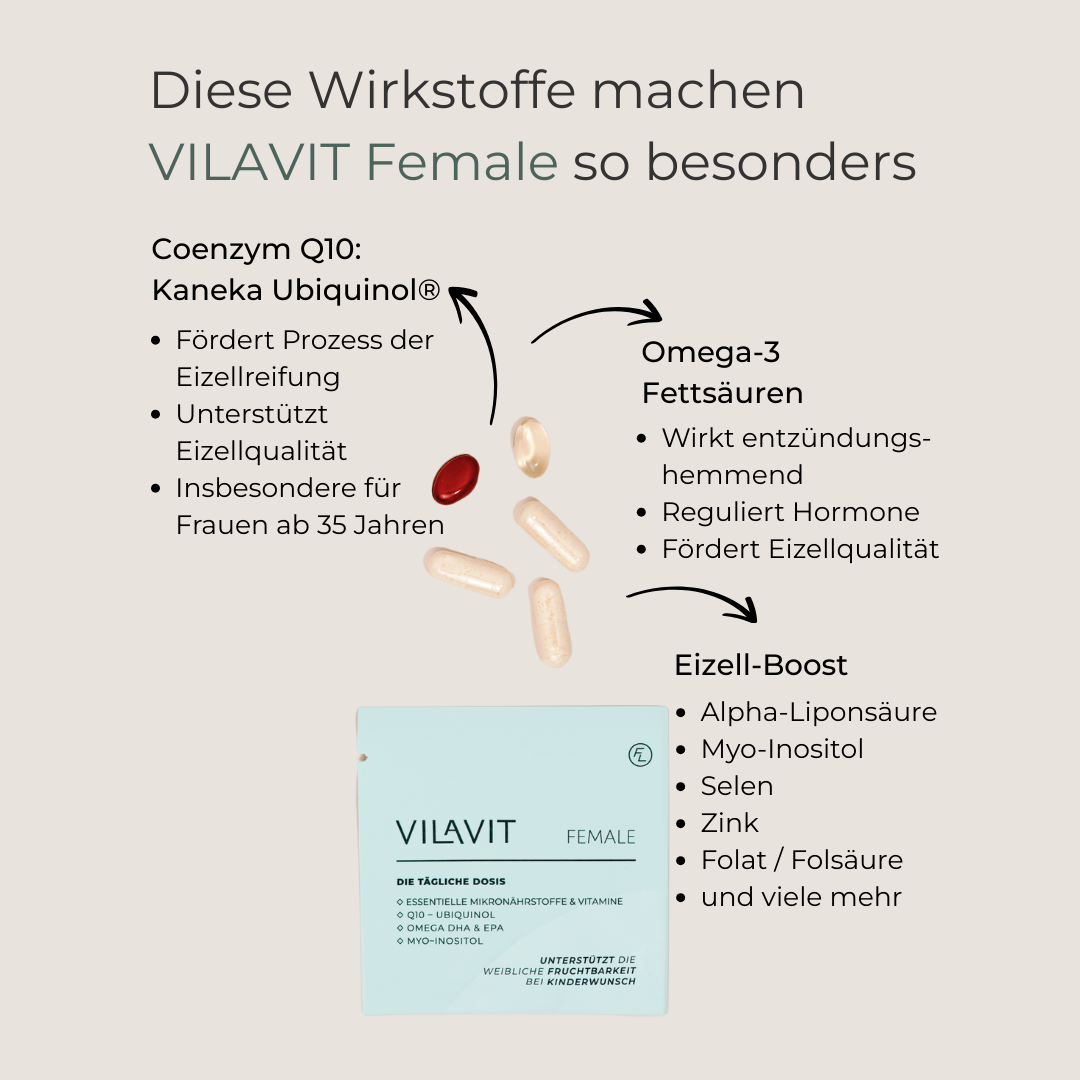
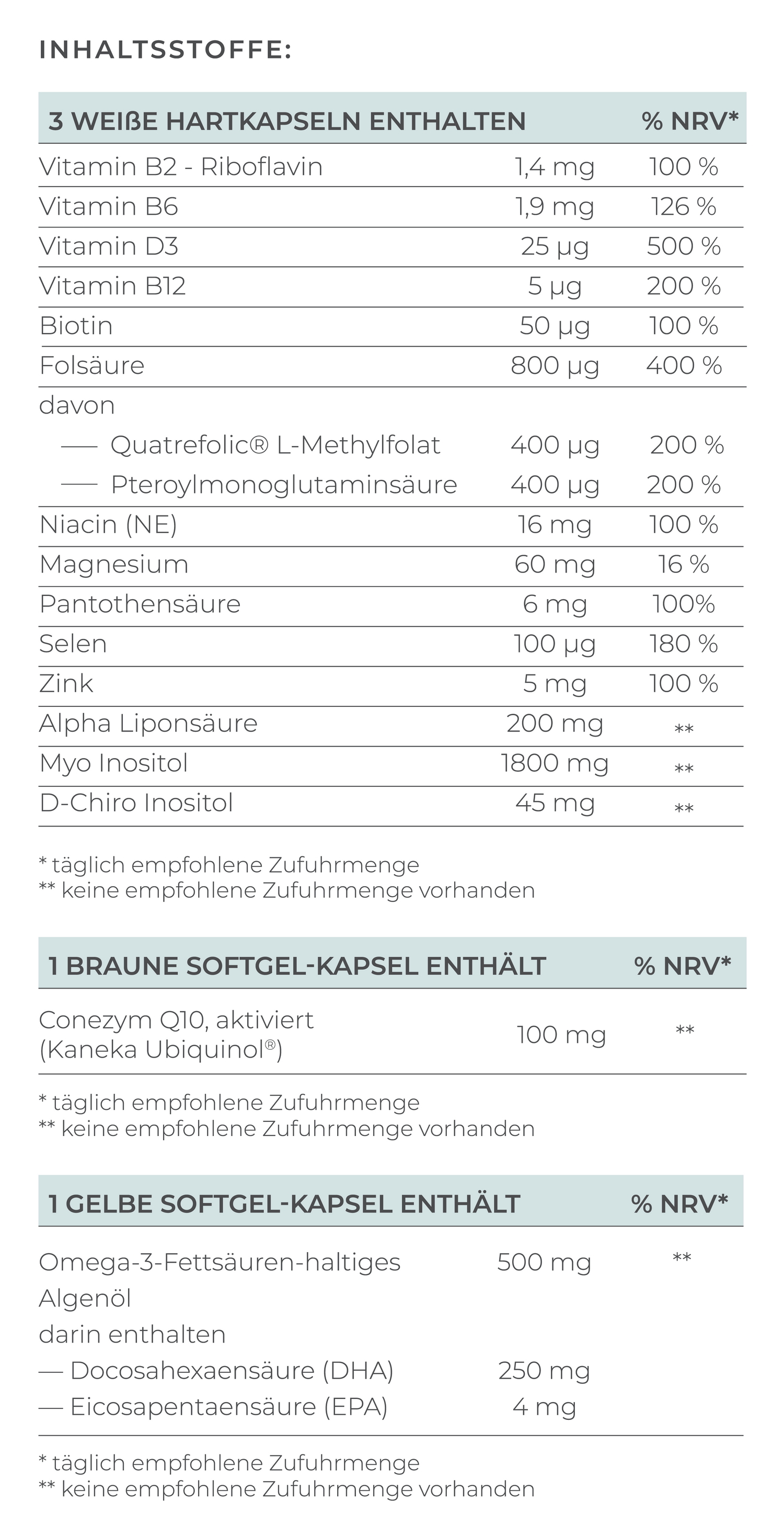
All treatment options require targeted supply of essential nutrients to enhance fertility and optimally prepare the female body for pregnancy. VILAVIT Female specifically promotes egg maturation and egg quality, thereby contributing to the improvement of embryo quality. Furthermore, VILAVIT Female supports the restoration of a regular cycle with ovulation.
Our VILAVIT product range was developed by a team of experts and combines all important micronutrients to ensure comprehensive and effective support of egg and embryo quality.










VILAVIT Female
- Regular price
-
€69,00 - Regular price
-
- Sale price
-
€69,00
Usage
Experts recommend starting to take VILAVIT Female at least three months before the planned conception. Since the maturation of an egg takes about 3 to 4 months, early supplementation with targeted micronutrients can help optimally support this sensitive process and improve the conditions for a successful conception.
Recommended Intake
Take one sachet daily (equivalent to 5 capsules).
Open the sachet and swallow each capsule individually with plenty of water.
Not suitable for children and adolescents.
Our Quality Promise
- Manufactured according to the highest quality and production standards
- Reviewed by external experts
- Made in Austria