Key Points for Supporting Implantation at a Glance:
- Implantation ideally occurs between the 6th and 10th day after ovulation.
- The uterine lining should be at least 7-8 mm thick.
- Progesterone is essential for implantation, while estrogen actively helps build the uterine lining.
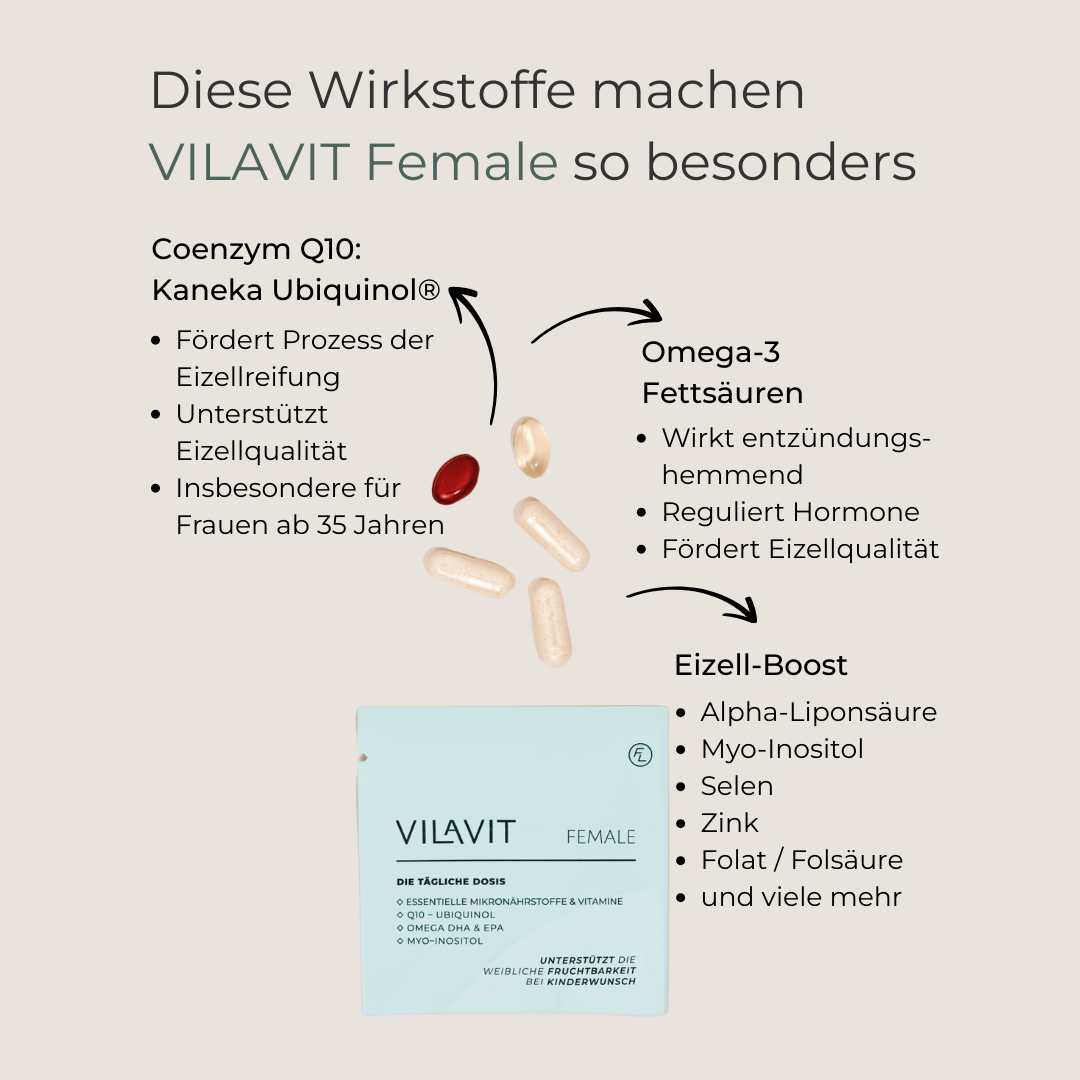
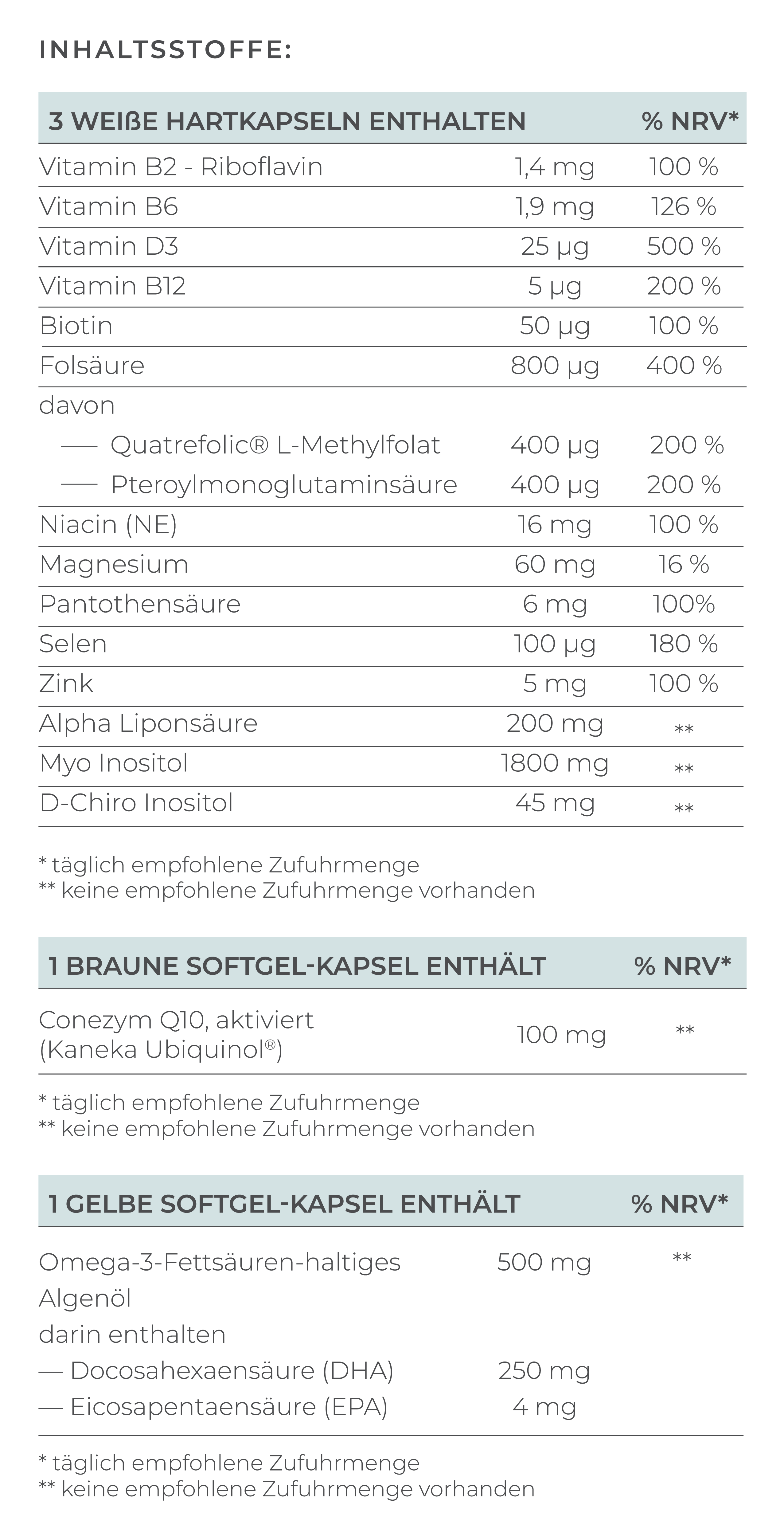
- Omega-3 fatty acids, vitamin D, folic acid, selenium, niacin, and vitamin B2 support implantation.
- In some cases, medications like immunosuppressants, cortisone, progesterone, hCG, aspirin, and heparin may assist in implantation.
Important Conditions for Implantation
Implantation, also known as nidation, is a crucial process where the fertilized egg, or embryo, embeds itself in the uterine lining (endometrium). It’s a highly complex process that depends on both the quality of the embryo and the receptivity of the uterine lining. Both factors must be perfectly synchronized to fulfill your desire for a child.
Implantation Window
The implantation window for embryos is between the 6th and 10th day after ovulation. This period is seen as the optimal phase for implantation, as the uterine lining is ideally developed to allow the fertilized egg to attach. The hormone progesterone, produced by the ovaries, makes the uterine lining receptive during this time. Before that, estrogen helps the lining grow.
Well-Developed Uterine Lining
For successful implantation, the uterine lining must be well developed. The ideal thickness varies, but generally, a thickness of at least 7 to 8 millimeters is considered favorable (Saad-Nagulb, 2020). Some experts even recommend a thickness of 9 millimeters or more for optimal implantation conditions (Soliman, 2008).
It's also important that the endometrium is three-layered. Each layer has its own function, and if one layer doesn’t work properly, it can negatively affect the chances of pregnancy:
- Basal Layer: Provides a stable foundation for regeneration and ensures continuous supply of nutrients and growth factors.
- Functional Layer: Offers a thick, well-vascularized layer rich in nutrients and proteins essential for the embryo’s survival and growth.
- Basal Lamina: Maintains the structure and function of the lining and plays a role in interactions between the lining and the embryo during implantation.
Embryo Quality
The quality of the embryo is critical for successful implantation and depends on both egg quality and sperm quality. Features that indicate embryo quality include:
- Cell number and symmetry
- Cell morphology: Healthy embryos have normally shaped cells with intact membranes and even distribution of the cell nucleus.
- Fragmentation: Low fragmentation, or few broken cell parts, is a sign of good embryo quality. High fragmentation may indicate cell damage and reduce implantation chances.
- Genetic integrity: The genetic integrity of the embryo is crucial for its viability and implantation potential. Embryos with a normal chromosome count and no genetic anomalies have a higher likelihood of successful implantation and a healthy pregnancy.
- Implantation potential: Some IVF clinics use advanced assessment methods like time-lapse imaging and genetic testing to evaluate an embryo's implantation potential, helping select those with the highest chances.
The Gardner Embryo/Blastocyst Grading System is a common method used by embryologists to evaluate embryo quality and determine its development and potential success. This system uses a combination of a letter and two numbers (e.g., 4AA, 2BA, 5AB).
Gardner Embryo/Blastocyst Grading System: The Numbers
The number (1-6) represents the developmental stage of the blastocyst or the degree of cavity expansion in the embryo (5 being the best).
- Early blastocyst – The embryonic cavity (blastocoel) is less than half the volume of the embryo.
- Blastocyst – The blastocoel is greater than or equal to half the volume of the embryo.
- Full blastocyst – The blastocoel completely fills the embryo.
- Expanded blastocyst – The blastocoel volume is greater than that of the early embryo, and the zona pellucida is thinning.
- Hatching blastocyst – The trophectoderm has begun breaking through the zona pellucida.
- Hatched blastocyst – The blastocyst has completely left the zona pellucida.
Gardner Embryo/Blastocyst Grading System: The Letters
Following the number, two letters represent two parts of the embryo on day 5 (blastocyst stage):
- First letter: Quality of the inner cell mass (ICM), which will become the fetus. A – C (A is the best).
- Second letter: Quality of the trophectoderm cells (TE), which will become the placenta. A – C (A is the best).
Possible Causes of Implantation Failure
The implantation process is one of the most complex steps toward a successful pregnancy. Several factors can lead to implantation failure, including:
- Hormonal imbalances or luteal phase defects
- Structural problems with the uterus or endometrium, such as polyps or fibroids
- Adhesions, possibly from endometriosis
- Nutrient deficiencies
- Poor embryo development or failure to hatch
- Timing issues with implantation
- Problems in the signaling between mother and child
- Immune reactions, such as high levels of natural killer (NK) cells
- Unhealthy habits like smoking and excessive alcohol consumption
How to Support Implantation
Medications:
- Immunosuppressants: Often used to suppress the body’s immune response, especially in cases with high levels of NK cells. NK cells, part of the immune system, can sometimes attack embryos as foreign bodies. Immunosuppressants help reduce this response, increasing the chance of a successful pregnancy.
- Cortisone: Cortisone has an immunosuppressive effect and can also reduce inflammation that might impede implantation.
- Intralipid infusions: Intralipid, a fat emulsion administered intravenously, has anti-inflammatory effects. It can promote implantation by reducing NK cell activity and making the uterine lining more receptive.
Hormonal Support:
- Progesterone: Fertility clinics often administer progesterone after ovulation to support the uterine lining and promote implantation. It can be given as tablets, capsules, suppositories, or injections.
- hCG (human chorionic gonadotropin): hCG, produced by the embryo during pregnancy, supports implantation and the continuation of pregnancy. In some cases, hCG can be artificially administered to promote implantation.
Blood-Thinning Agents:
- Aspirin (low dose): Aspirin has a blood-thinning effect and can improve blood flow to the uterine lining, supporting implantation, especially in women with clotting disorders.
- Heparin: A stronger blood-thinner, usually given only to women with diagnosed clotting disorders.
Implantation Flush: Before an embryo transfer, an implantation flush involves rinsing the uterine cavity with a special nutrient solution to prepare the uterine lining for implantation.
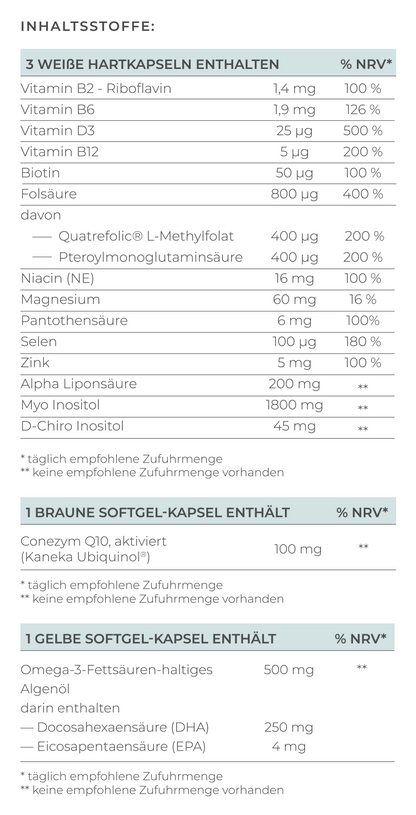
Micronutrients:
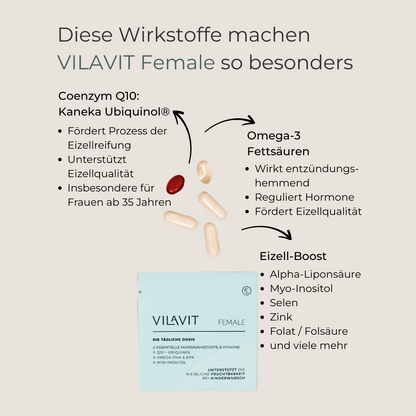
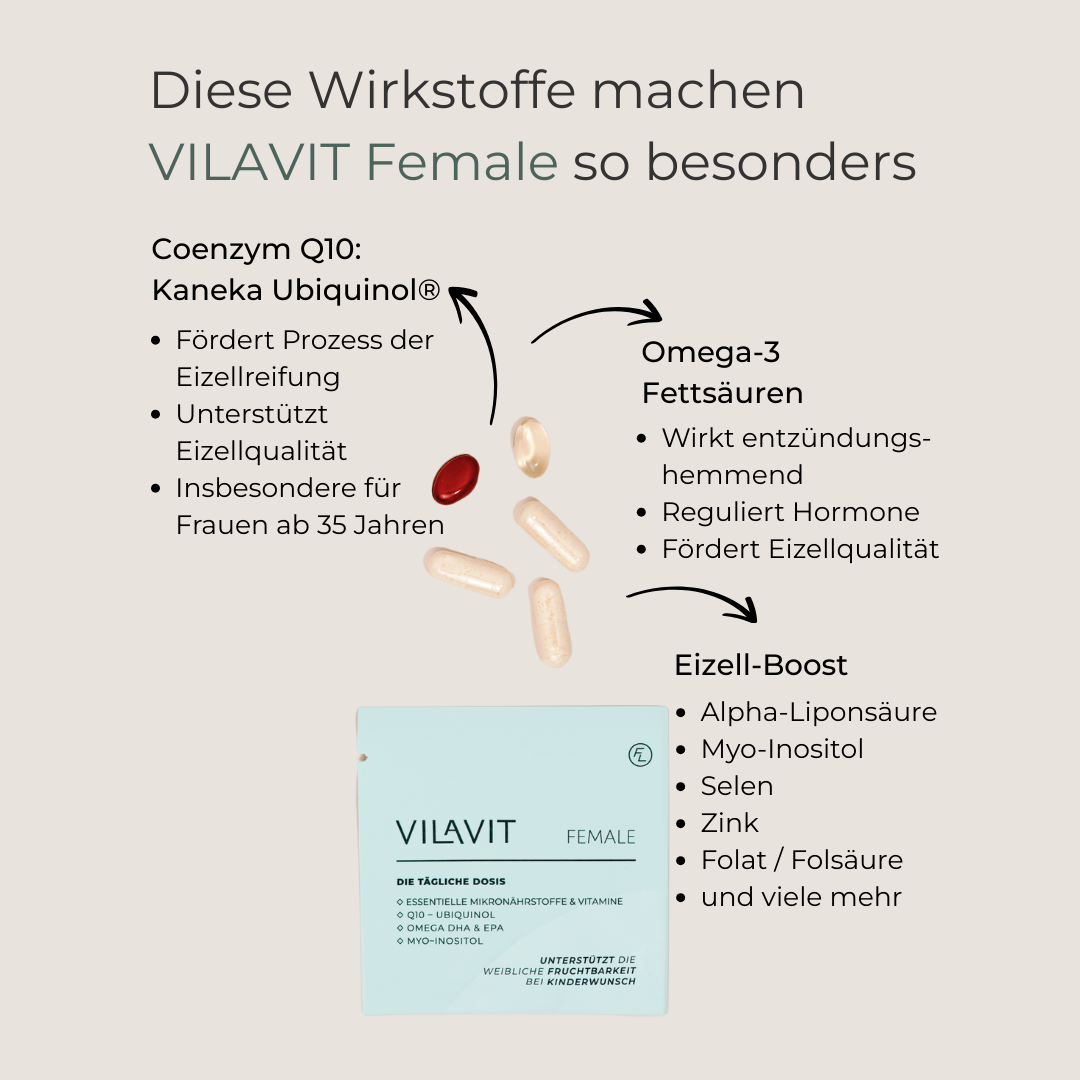
- Omega-3 fatty acids: Omega-3s, especially DHA, help regulate the immune system. High NK cell levels can negatively impact implantation, and DHA’s anti-inflammatory effect can help reduce this response, increasing implantation chances.
- Vitamin D: A deficiency in vitamin D is linked to reduced implantation ability. Vitamin D plays an important role in regulating the immune system and inflammation, crucial for successful implantation.
- Folic Acid (Vitamin B9): Known for its role in neural tube development, folic acid can also support implantation by promoting blood supply and improving the uterine lining.
- Selenium: Selenium’s antioxidant properties contribute to egg quality, which is important for fertilization and implantation.
- Niacin and Vitamin B2: These micronutrients support the formation and maintenance of the uterine lining.
Additional Tips to Promote Implantation
- Reduce stress: Chronic stress can negatively impact the reproductive process, including implantation. Relaxation techniques such as yoga, meditation, and breathing exercises can help reduce stress and increase the chances of successful implantation.
- Healthy diet: A balanced diet rich in fruits, vegetables, whole grains, lean protein, and healthy fats can support overall health and the uterine lining’s readiness for implantation.
- Avoid smoking and excessive alcohol consumption: These habits can negatively affect female fertility. Studies show that toxins in tobacco can impair the uterine lining's development. Men should also avoid smoking, as it reduces sperm quality.
Conclusion: Implantation is a Complex Process
In summary, implantation is a complex process influenced by many factors. By maintaining a healthy lifestyle, balanced nutrition, stress management, and targeted micronutrient supplementation, the likelihood of successful implantation can be increased. The implantation phase can be emotionally challenging, especially for couples experiencing infertility. However, it is important to consult a specialist if implantation failure persists or concerns arise, to undergo necessary tests and receive the appropriate treatment recommendations. If you are currently undergoing fertility treatment or about to start your IVF or ICSI, you should ask your doctor about ways to support implantation. Supplements can also be useful to support the quality of eggs and sperm, thus increasing the chances of successful implantation.
FAQ
How do I know if implantation was successful?
The only sure sign of successful implantation is a positive pregnancy test: A pregnancy test detects the hormone hCG (human chorionic gonadotropin) in the urine or blood. hCG is only produced after successful implantation by the developing placenta. Therefore, a positive test is the most reliable evidence of pregnancy.
Other possible (uncertain) signs include:
- Implantation bleeding: Some women notice light bleeding or spotting at the time of implantation. This occurs when the embryo implants into the uterine lining. Implantation bleeding is usually lighter than menstrual bleeding and often has a bright red or brownish color.
Important: Not every woman experiences implantation bleeding, and not every bleeding at this time is implantation bleeding. - Implantation cramps: Some women experience mild cramping or twinges in the lower abdomen during implantation. These cramps are also not a definitive sign and can have other causes, such as ovulation or premenstrual symptoms.
- Breast changes: Due to hormonal changes after implantation, the breasts may become more sensitive, swollen, or feel tender.
- Fatigue and exhaustion: Many women feel tired and exhausted in early pregnancy.
- Nausea: Morning sickness, particularly nausea, can be an early sign of pregnancy.
- Heightened sense of smell: Some women become more sensitive to smells in early pregnancy.
- Changes in cervical mucus: After implantation, cervical mucus can become thicker and creamier. Your body also produces more cervical mucus during pregnancy.
How long does implantation take?
Implantation takes about 6 to 10 days from fertilization to complete implantation. The following processes occur in the body:
- Day 1: The fertilized egg (zygote) begins to divide while traveling through the fallopian tube.
- Days 5-6: The egg reaches the uterine cavity and is referred to as a blastocyst.
- Days 6-10: The blastocyst begins to implant into the uterine lining.
- Days 10-12: Implantation is complete when the blastocyst is fully embedded in the uterine lining.
When is implantation complete?
Implantation is complete when the blastocyst is fully embedded in the uterine lining and starts producing hCG. This usually happens around the 10th to 12th day after fertilization.
Implantation did not succeed. What can I do?
If implantation fails after artificial insemination or early miscarriage occurs, it can be very stressful. In this case, it is important to determine the causes precisely. Tests may include examination of the uterine cavity, genetic testing of the embryos, as well as immunological and coagulation tests.
The treatment plan can then be adjusted accordingly, for example, by modifying hormone therapy, using immunosuppressants or anticoagulants, or supporting implantation with Assisted Hatching (AHA) or EmbryoGlue.
Possible treatment options to increase your chances of implantation include:
- Optimizing the uterine lining: Hormonal treatment with estrogen and progesterone, surgical removal of fibroids or polyps, or laparoscopy to diagnose and treat endometriosis.
- Improving egg and embryo quality: Adjusting lifestyle and using supplements.
- Immunological therapy: Using immunosuppressants (e.g., corticosteroids) or Intralipid infusions.
- Treating coagulation disorders: With blood thinners (e.g., aspirin, heparin).
- Hormonal therapy: Using progesterone supplementation and treating any thyroid disorders.
Implantation succeeded, but I had an early miscarriage.
If you have experienced an early miscarriage after artificial insemination, it is very distressing. In this case, it is important to investigate the causes in order to improve your chances in future attempts.
The following measures may help:
- Comprehensive diagnostics: Examination of the uterine cavity (hysteroscopy), immunological diagnostics, genetic testing of both partners, and coagulation diagnostics.
- Adjusting the treatment plan: Modifying hormonal stimulation, using immunosuppressants or anticoagulants, and supportive measures at the fertility clinic (Assisted Hatching, EmbryoGlue, implantation wash).
- Genetic testing of the embryo: If possible, a genetic test of the embryo (e.g., after a miscarriage) can provide information about potential chromosomal abnormalities that may have caused the miscarriage.
- Infection screening: Certain infections can increase the risk of miscarriage. It is advisable to test for infections such as toxoplasmosis, rubella, cytomegalovirus, and herpes.
- Sperm analysis: The quality of sperm may also play a role. A new sperm analysis of the partner may be helpful.
- Thyroid function analysis: Thyroid disorders (such as Hashimoto's thyroiditis) can influence fertility and increase the risk of miscarriage.
References
Heger et al. Rauchen verringert die Endometriumdicke bei IVF/ICSI-Patientinnen. Thieme, 2018.