Fertility Treatments for Endometriosis
Success Rates
Success rates depend on the stage of endometriosis, the woman's age, egg reserve, sperm quality, the experience of the fertility center, and other factors.
Studies show that IVF is often successful in women with endometriosis, especially when endometriosis lesions have been removed beforehand (Zhong, 2021).
The chances of pregnancy are highest when the woman is younger than 35 years old and has only mild endometriosis (Morcel, 2024).
How Can I Get Pregnant with Endometriosis?
The good news: Getting pregnant with endometriosis is possible!
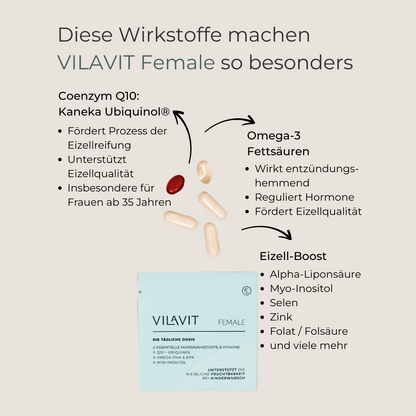
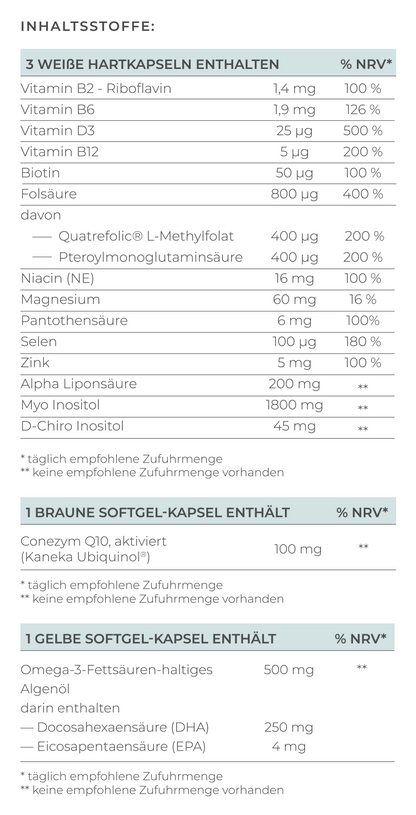
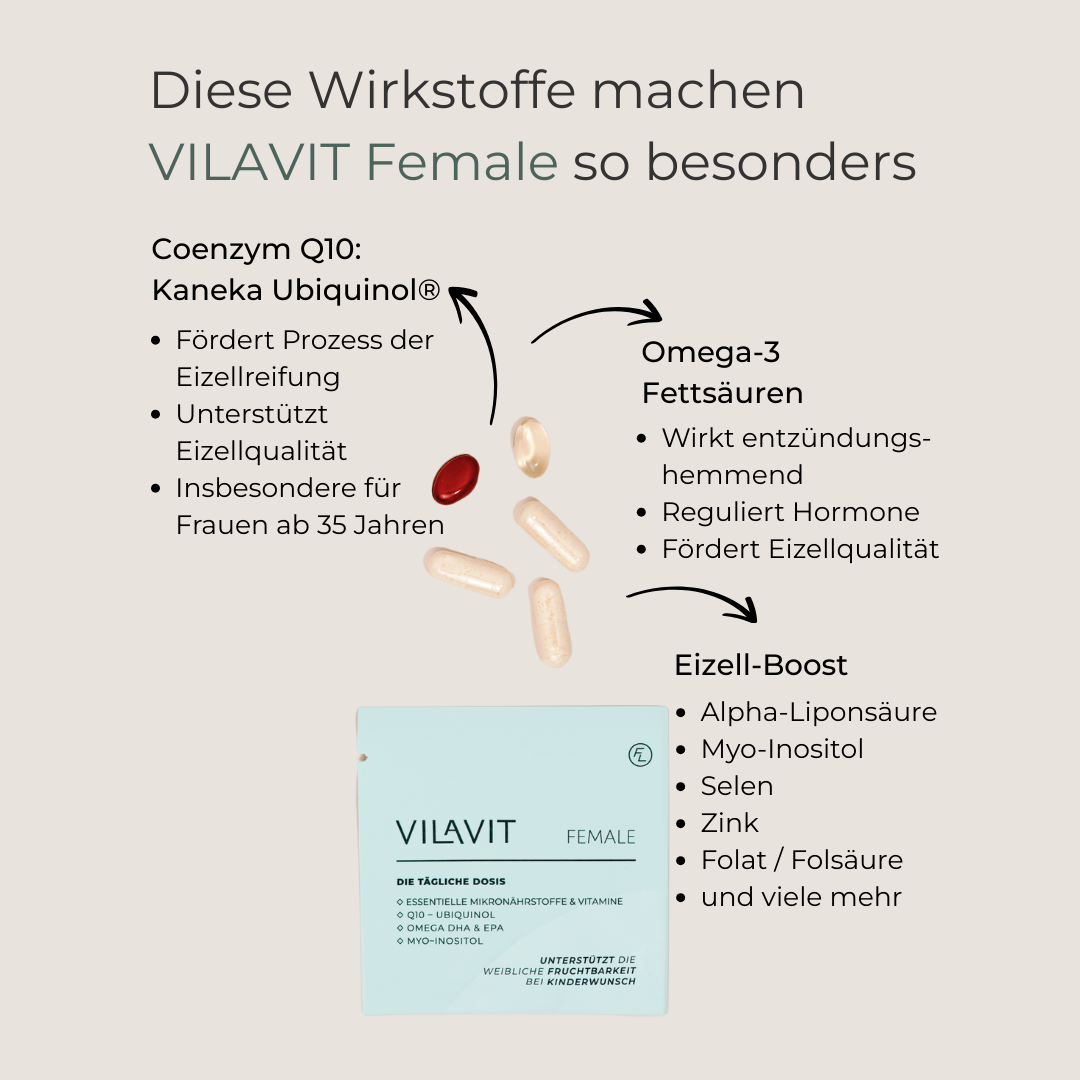
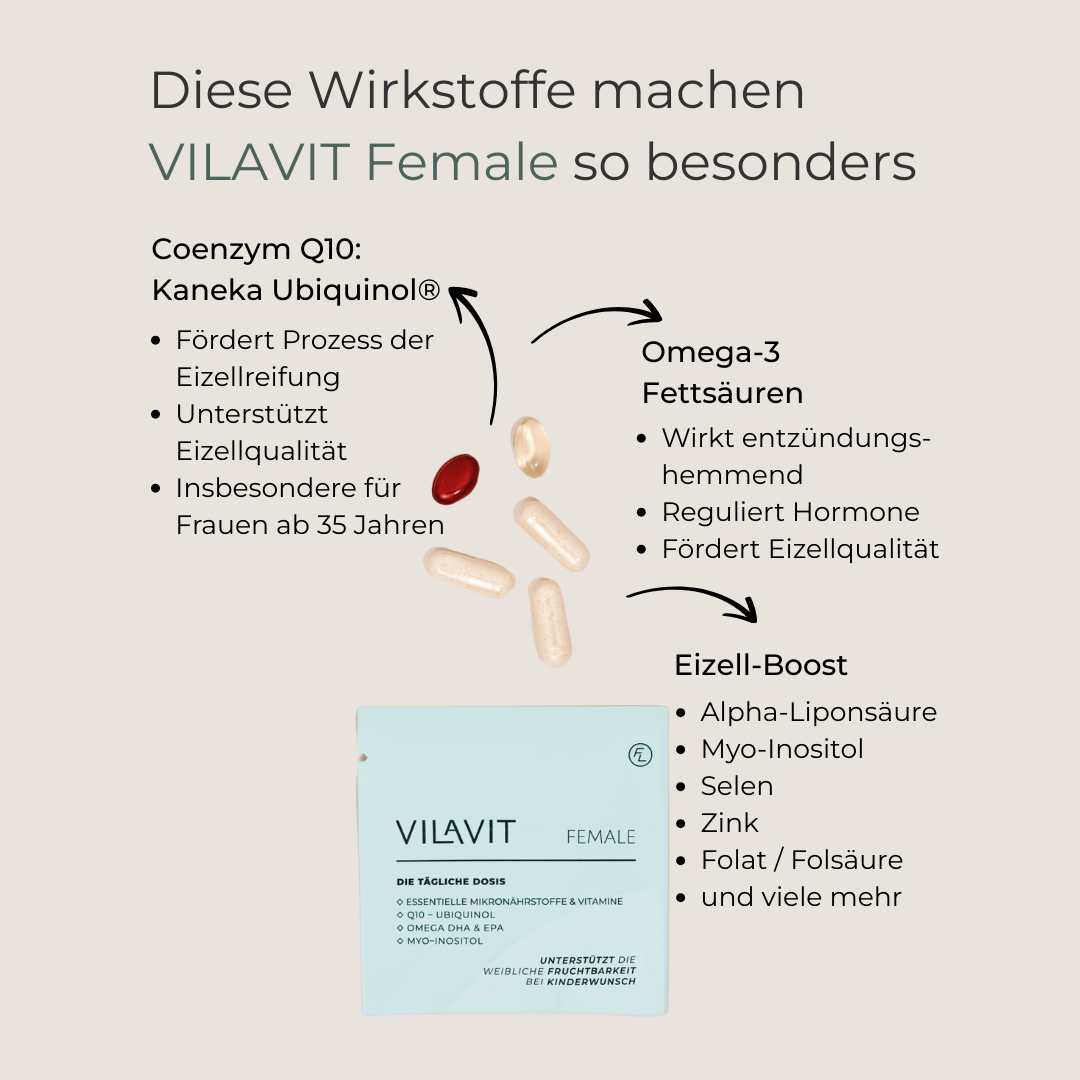
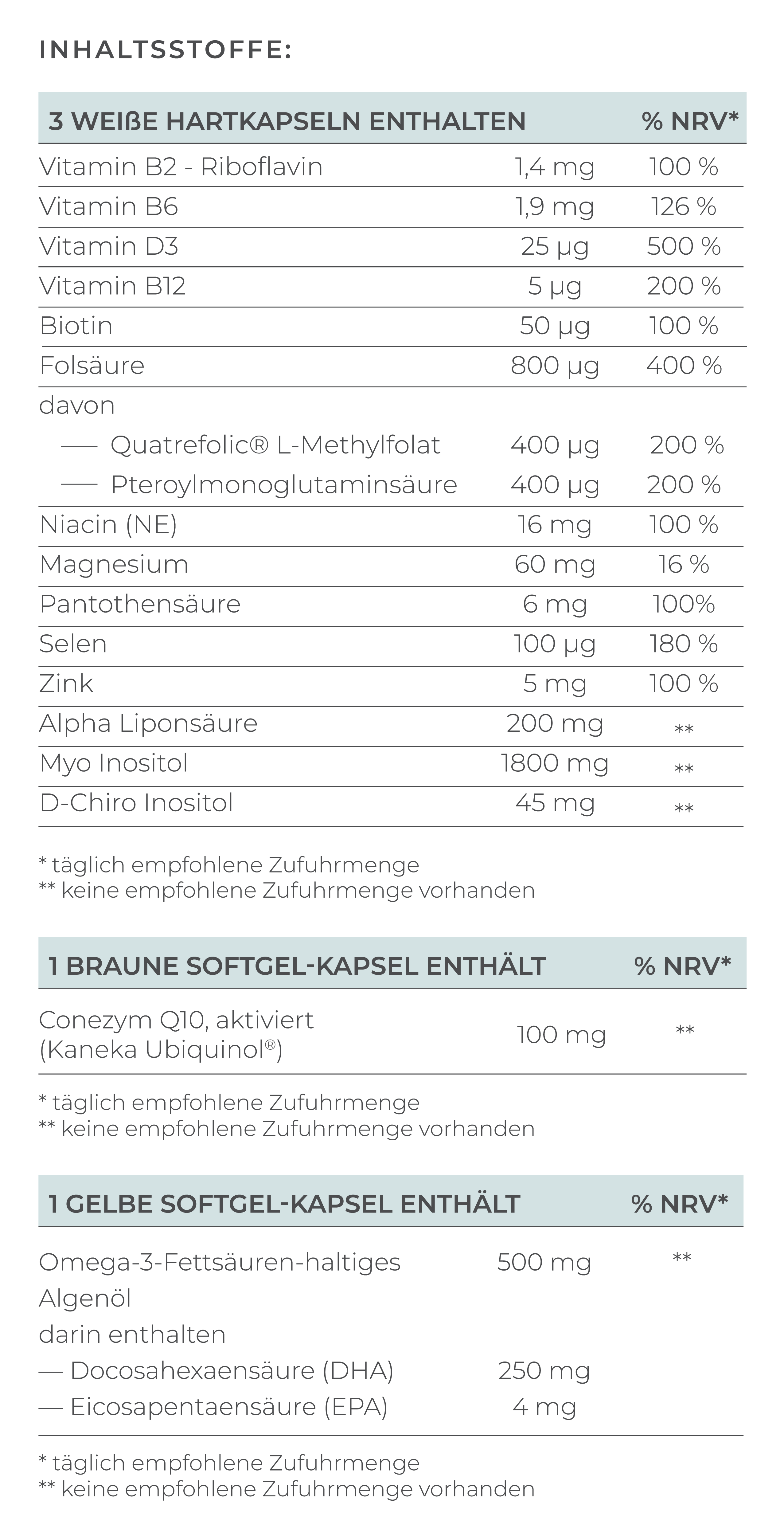
In addition to medical treatment, scientific studies have shown that certain nutrients can improve egg quality even in women with endometriosis. Essential nutrients include Coenzyme Q10 in the form of ubiquinol, vitamin D, omega-3 fatty acids, and numerous antioxidants such as alpha-lipoic acid (Hart, 2024).
A healthy and active lifestyle is also important, as well as avoiding stress, smoking, and excessive alcohol consumption.
Endometriosis may complicate the path to parenthood, but it cannot completely block it. Thanks to advances in reproductive medicine, there is hope and ways to realize the dream of becoming a parent, even with this challenging condition.
Conclusion
Endometriosis is a complex condition that affects the fertility of many women. However, advances in diagnosis and treatment, especially in reproductive medicine, offer hope and realistic chances of pregnancy. Early diagnosis and individualized treatment, combined with a healthy lifestyle, balanced anti-inflammatory diet, and adequate supply of high-quality micronutrients that support egg quality, pave the way to parenthood.
FAQ
What are typical symptoms of endometriosis?
Typical symptoms of endometriosis can vary widely from mild to severe. The severity of symptoms does not always correlate with the severity of endometriosis. Some women have few or no symptoms despite having extensive endometriosis, while others with milder forms may be severely affected. Common symptoms include cyclic pain, occurring around the time of menstruation.
The most common signs include:
- Severe menstrual pain (dysmenorrhea)
- Chronic pelvic pain
- Pain during intercourse (dyspareunia)
- Painful urination
- Painful bowel movements
- Heavy or prolonged bleeding (menorrhagia)
- Spotting between periods
- Bloating and abdominal pain (endo-belly)
- Nausea or digestive problems
- Fatigue and tiredness
Can endometriosis recur after laparoscopy?
Yes, endometriosis can recur after laparoscopy.Studies show that in about 20-50% of women, endometriosis reoccurs within 5 years after surgery (Guo, 2009).Without hormonal follow-up treatment, remaining or newly developed lesions can be reactivated by menstrual cycles.Women with severe endometriosis (Stage III or IV) have a higher risk of recurrence.What causes endometriosis?
The causes of endometriosis and its exact mechanisms are not fully understood. Various factors likely play a role, such as retrograde menstruation, genetic predisposition, a changed immune system, and hormonal influences. Environmental factors might also increase the risk of endometriosis. Research is actively working to better understand the causes and develop new treatment options.
How can recurrence be prevented?
Surgical therapy combined with hormonal treatment (e.g., progestins or GnRH analogs) can reduce the risk of recurrence.Continuous use of hormonal contraceptives (e.g., the pill) can inhibit the growth of endometriosis lesions.Women with endometriosis should have regular check-ups with their gynecologist or at a specialized endometriosis center to detect potential recurrences early.
Do women with endometriosis have a higher risk of miscarriage?
Yes, studies suggest that the risk of miscarriage is higher in patients with endometriosis. A meta-analysis involving over 50,000 women found that the miscarriage risk in pregnant women with endometriosis was 35.8%, compared to 22% in women without endometriosis (Kohl Schwartz, 2017).References
Zhong et al. Analysis of IVF/ICSI Outcomes in Endometriosis Patients With Recurrent Implantation Failure: Influence on Cumulative Live Birth Rate. Frontiers in Endocrinology, 2021.
Morcel et al. What is the impact of endometriosis and the AFS stage on cumulative pregnancy rates in IVF programs? Reproductive Health, 2024.
Bulletti et al. Endometriosis and infertility. Journal of Assisted Reproduction and Genetics, 2010.
Hart, Roger J. Nutritional supplements and IVF: an evidence-based approach. Reproductive Biomedicine Online, 2024.
Guo, Sun-Wei. Recurrence of endometriosis and its control. Human Reproduction Update, 2009.
Kohl Schwarz et al. Endometriosis, especially mild disease: a risk factor for miscarriages. Fertility and Sterility, 2017.