Everything you need to know about getting pregnant after a miscarriage
-
Around 43% of women who have already had a child have experienced at least one miscarriage.
-
The risk of another miscarriage is not higher after a single miscarriage.
-
Chromosomal abnormalities are the most common cause of miscarriage.
-
Examinations like blood tests, ultrasounds, or genetic analyses can help clarify the causes and support the next pregnancy.
-
The WHO recommends waiting 6 months, although studies show that getting pregnant earlier is often successful.
Miscarriages Are More Common Than You Think
A miscarriage (spontaneous abortion), the loss of a fetus before the 20th week of pregnancy, is one of the most common complications during early pregnancy.A study of over 50,000 women shows that around 43% of all women who have already had a child have experienced at least one miscarriage. (Cohain et al, 2017).
This number may actually be higher in reality, as many women experience a miscarriage before they even know they are pregnant.
Many women already take a pregnancy test when they suspect they might be pregnant, often before their period is even missed. A positive test triggers a variety of emotions. However, it's important to know that very early pregnancies, called biochemical pregnancies, often end unnoticed. These early miscarriages can often be mistaken for a late or heavier period.
The loss of a child can be a profound emotional and physical challenge, often raising questions, fears, and grief in the women affected. A common question is how and when one can get pregnant after a miscarriage.
Many women are afraid of a new pregnancy after a miscarriage. In most cases, the risk of another miscarriage is not increased.
Causes of Miscarriage
There are many possible causes of miscarriage. It's important to know that neither you nor your partner are to blame. In most cases, a miscarriage is due to chromosomal abnormalities.
Chromosomal Abnormalities
The most common cause of miscarriage is chromosomal abnormalities in the embryo. At least 50% of all miscarriages in the first trimester are caused by chromosomal abnormalities. (Melo et al., 2023)
These abnormalities often occur randomly during fertilization or cell division, causing the embryo to develop abnormally.
The risk of chromosomal disorders also increases with the age of the parents, particularly the mother, but also the father.
This is because the quality of eggs, and to some extent sperm, declines with age, which increases the chances of chromosomal misdistribution, such as with Down syndrome, especially from age 35 onward.
Hormonal Imbalances
Hormonal imbalances, especially luteal phase defects, thyroid dysfunctions, and polycystic ovary syndrome (PCOS), can lead to miscarriages.
Anatomical Anomalies
Structural abnormalities or adhesions in the uterus can increase the risk of habitual miscarriage. These can usually be identified via ultrasound, hysteroscopy, or laparoscopy.
Infections
Certain bacterial infections, such as toxoplasmosis, can lead to miscarriage by damaging the placenta or fetus.
Immunological Causes
The immune system can reject tissue characteristics inherited from the father, thus preventing a successful pregnancy.
Thrombophilia (Blood Clotting Disorders)
The Factor V Leiden mutation can lead to vessel blockages. Microthrombosis can prevent an embryo from implanting successfully.
Chronic Maternal Diseases
Diabetes, high blood pressure, or autoimmune diseases in the mother can increase the risk of miscarriage.
Placental Abnormalities
The placenta plays a crucial role in supplying oxygen and nutrients to the fetus. Structural or functional disorders of the placenta can lead to inadequate supply and increase the risk of late miscarriage. Relevant conditions and diseases include:-
Placental insufficiency: Inadequate placenta function can impair fetal growth.
-
Placenta previa: A low-lying placenta can lead to bleeding and endanger the baby’s supply.
-
Placental abruption (Abruptio placentae): Premature detachment of the placenta can cause life-threatening complications for both the mother and child.
-
Placental infarction: Small blood clots in the placenta can reduce circulation and increase the risk of miscarriage.
Cervical Insufficiency (Cervical Weakness)
A weak cervix can cause premature dilation.
Preeclampsia
This pregnancy-related condition with high blood pressure and protein in the urine can lead to severe complications.
Uterine Infections (Chorioamnionitis)
Bacterial infections can damage the amniotic fluid and placenta.
Lifestyle Factors
Smoking, excessive alcohol consumption, drug use, and certain environmental factors like radiation, chemicals, and pesticides can also increase the risk of miscarriage.
Miscarriages Without Identifiable Causes
Sometimes no medical reason for a miscarriage can be identified.
What happens in the body after a Miscarriage?
1. Hormonal Changes
During pregnancy, the body produces high amounts of pregnancy hormones such as hCG (human chorionic gonadotropin), progesterone, and estrogen. After a miscarriage, hCG levels gradually decrease, which can take several weeks. This hormonal drop can cause mood swings, fatigue, and other physical symptoms. The menstrual cycle usually resumes within four to six weeks.
2. Physical Reactions
After a miscarriage, heavy bleeding similar to a very strong period is common. This can last from a few days to weeks.The uterus contracts to expel tissue and the uterine lining. These contractions can be felt as painful cramps.
3. Emotional and Psychological Processing
In addition to the physical changes, a miscarriage can trigger strong emotional reactions, including grief, guilt, or fear of another pregnancy. The hormonal drop can further intensify these feelings. Support from professionals, family, or support groups can be helpful during this phase.
If symptoms like persistent severe pain, fever, or excessive bleeding occur after a miscarriage, immediate medical attention should be sought.
Getting Pregnant After a Miscarriage
The loss of a child can bring deep sadness and uncertainty, but it’s important to know that a subsequent pregnancy is possible. Many women are able to carry a healthy pregnancy after a miscarriage. Certain medical tests can help ensure that there are no barriers to a successful pregnancy.
Follow-Up Exam
A visit to your gynecologist is important to identify any potential complications for a subsequent pregnancy.
Curettage / D&C (Dilation and Curettage)
In some cases after a miscarriage, it may be necessary to remove remaining pregnancy tissue from the uterus. This can be done through a curettage (D&C) or suction abortion to prevent complications like infections or excessive bleeding.
Such a procedure is also necessary if the fetus is no longer viable but hasn’t been expelled naturally.
Curettage (D&C):
- During a curettage, the doctor uses a curette, a spoon-shaped instrument, to gently scrape the uterine lining and pregnancy tissue.
- This procedure is usually performed under general anesthesia.
Suction abortion (Vacuum Aspiration):
- Suction is another common method in which a thin tube is inserted into the uterus to gently suck out tissue.
- This procedure can be done under local anesthesia, sedation, or general anesthesia.
- Suction abortion is often the common method in early pregnancy stages.
A blood test plays a crucial role in diagnosing the cause.
It can provide insight into the following:
HCG (human chorionic gonadotropin): HCG is the pregnancy hormone produced during pregnancy. An increase in HCG levels in the early weeks is crucial, while a decrease may indicate a miscarriage. Monitoring the HCG level helps doctors assess if the miscarriage is complete and whether pregnancy tissue remains in the uterus.
Progesterone: Progesterone is necessary to sustain the pregnancy. A low progesterone level may indicate that the body didn’t adequately support the pregnancy.
- Rh incompatibility
If an Rh-negative woman carries an Rh-positive child, her immune system may produce antibodies against the Rh-positive red blood cells of the fetus if the blood of the fetus comes in contact with the mother’s blood. This can especially happen after a miscarriage.
These antibodies can be dangerous in future pregnancies. If the mother has produced antibodies, they can attack the fetus’s blood, leading to severe health problems for the child.
- Detection of Infections and Autoimmune Diseases
Possible infections or autoimmune diseases in the mother can be the cause of a miscarriage.
- Nutrient Deficiencies
A lack of important nutrients like vitamin D or folic acid can impact fertility and the ability to maintain a pregnancy.
- Genetic Diagnostics
Blood tests of the parents for genetic abnormalities can provide insight, especially if multiple miscarriages have occurred.
In such cases, embryos can be tested for genetic abnormalities during IVF treatment using preimplantation genetic diagnosis (PGD) before being transferred into the uterus.
Recommended Waiting Time Before Trying Again
After a miscarriage, many women wonder when the best time to try for another pregnancy is. Doctors recommend waiting at least one full menstrual cycle or up to three months before attempting another pregnancy. The World Health Organization even recommends waiting around 6 months.
However, there is no data to support these recommendations. On the contrary, a 2016 study showed that a shorter waiting time of 0-3 months led to higher live birth rates. (Schliep et al, 2016).
Waiting for a regular menstrual cycle can help determine the timing of ovulation and thus better predict the fertile days.
Healthy Lifestyle for Physical and Emotional Strength
The loss of a child, regardless of the pregnancy week, is a physical and emotional turning point in a woman's life. In addition to medical follow-up, it's important to consider lifestyle changes and the proper intake of micronutrients. These factors can support physical health and increase the chances of a successful future pregnancy.
Healthy Diet
A balanced diet is essential for promoting fertility. The following foods can support female fertility:
-
Fruits and vegetables: These are rich in antioxidants, vitamins, and minerals.
-
Whole grains: Whole grains like oatmeal, whole wheat bread, and brown rice are high in fiber and support digestion and blood sugar levels.
-
Protein sources: Lean meats, fish, legumes, nuts, and seeds provide essential amino acids and are important for cell repair and regeneration.
-
Fats: Healthy fats from avocados, nuts, seeds, and olive oil are important for hormone production and overall health.
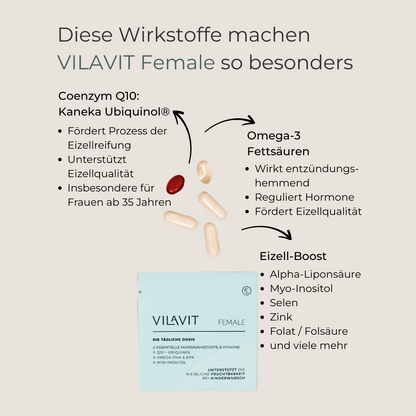
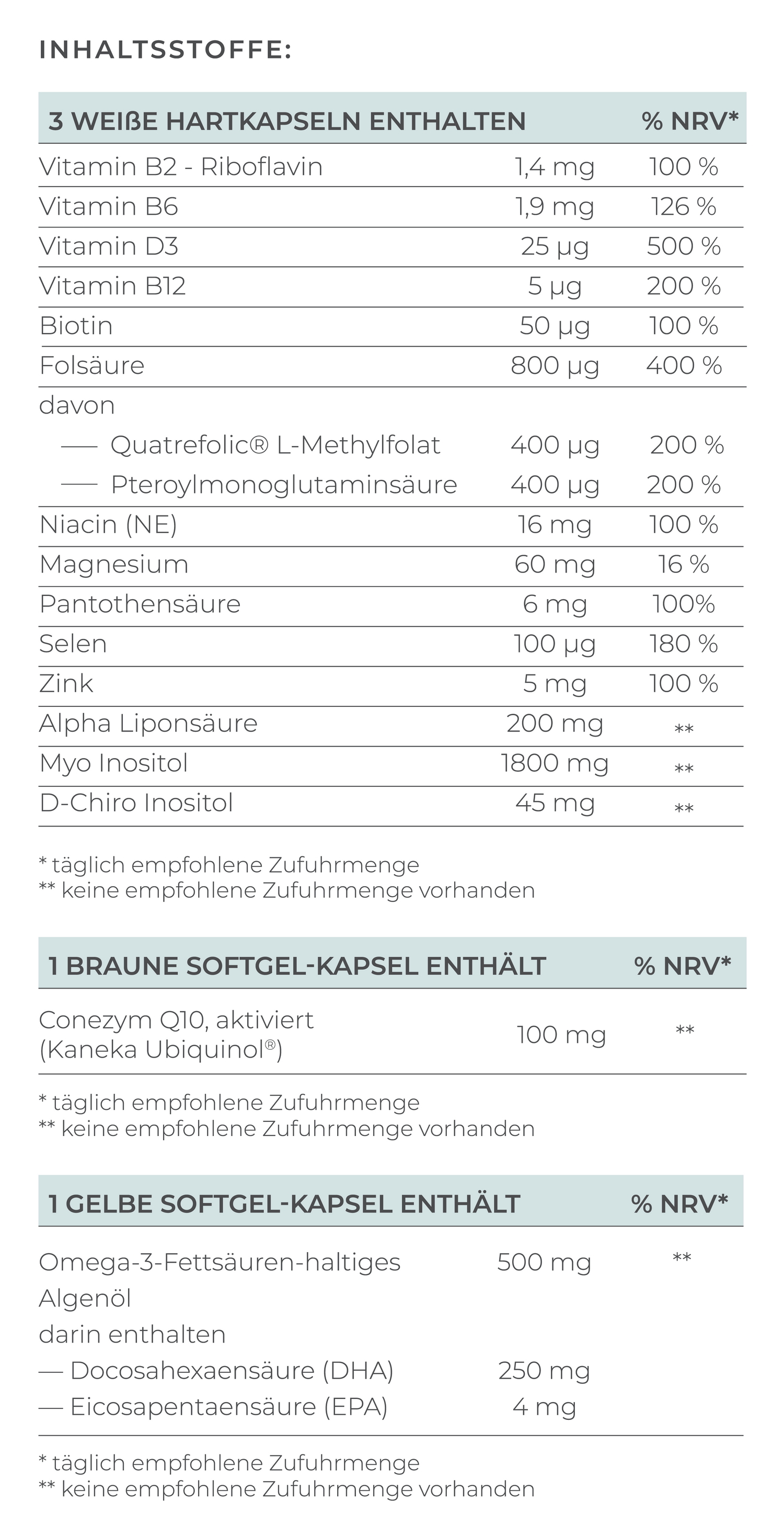
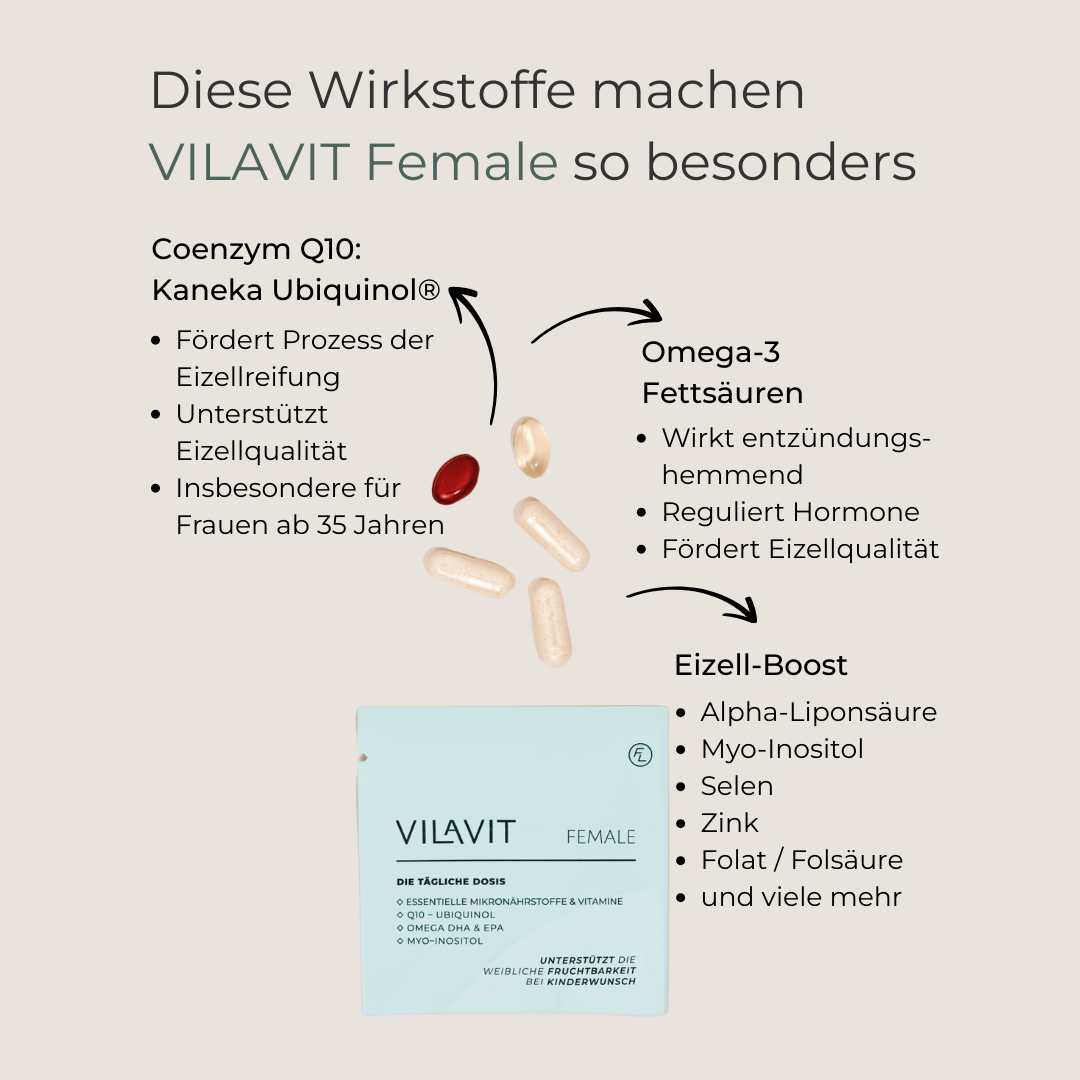
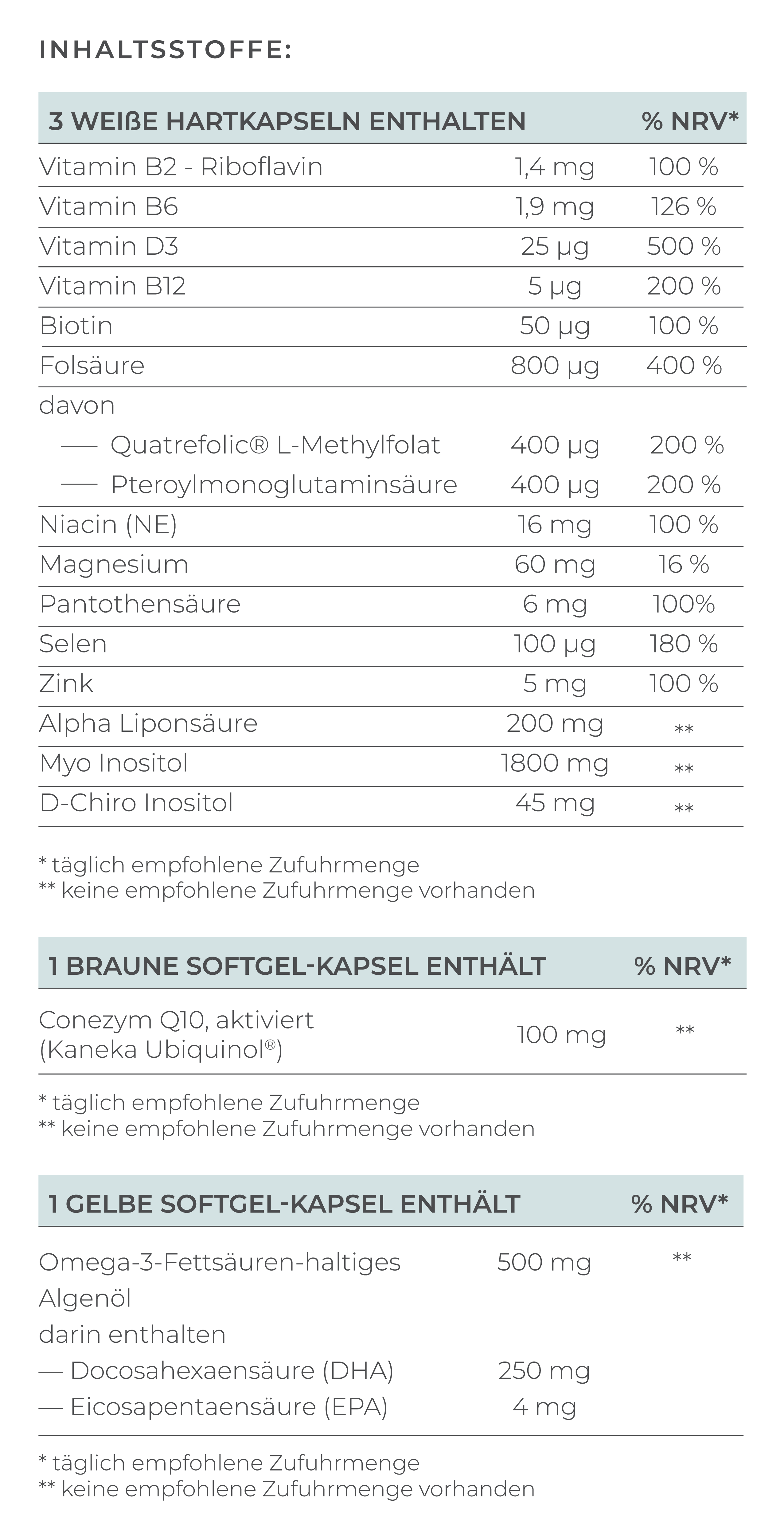
Micronutrients
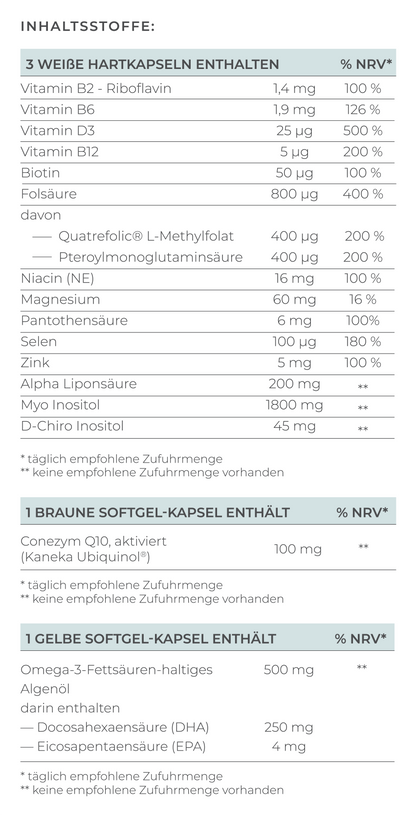
Taking certain micronutrients can improve egg quality and support the body during the healing process after a miscarriage. Here are some important nutrients to consider:-
Folic acid or Folate: Folic acid is essential for cell division and should be taken before pregnancy. However, around 50% of all women are unable to absorb folic acid, so the bioavailable form, folate, is recommended. Scientific studies have confirmed that taking folate is associated with a lower risk of miscarriage (Gaskins et al., 2014).
-
N-Acetyl-Cysteine (NAC): A study showed that women who took N-Acetyl-Cysteine (NAC) and folic acid were 2.9 times more likely to continue their pregnancy beyond the 20th week (Amin et al., 2008).
-
Vitamin D: Vitamin D plays an important role in female fertility. According to a 2022 study, women with a diagnosed vitamin D deficiency (<50 nmol/L) have an increased risk of miscarriage compared to women with sufficient vitamin D levels (Tamblyn et al., 2022).
Physical Activity
Regular physical activity not only supports physical health but also mental health. Moderate exercises such as walking, cycling, and yoga are recommended for stress management, along with strength training to strengthen muscles and improve overall fitness.
Psychological Support
Emotional health is just as important as physical health. Professional psychological counseling, support groups, and talking with close friends and family can help cope with grief and manage anxiety.
Stress Management
Stress can negatively affect fertility. The following techniques can help reduce stress:
-
Meditation and Mindfulness: Relaxation techniques such as meditation or yoga can promote inner calm and help stabilize emotional health.
-
Hobbies and Social Connections: Time for activities that bring joy, distract from the desire for children, and provide a supportive environment with loved ones.
Conclusion: Becoming Pregnant After a Miscarriage is Often Possible
Experiencing a miscarriage is a deeply painful experience, unfortunately much more common than many people realize. It is important to talk about it, as it is estimated that around 15% of all clinical pregnancies end in a miscarriage. Often, the cause is a chromosomal anomaly, a genetic change beyond the person's control. Therefore, a miscarriage is never the woman's fault.
The experience of a miscarriage can be physically and emotionally burdensome for affected women. Despite the grief, there is hope, as becoming pregnant after a miscarriage is possible.
Important steps include medical examinations to identify possible causes and determine necessary treatments. In addition, a balanced diet, the intake of micronutrients, regular physical activity, and stress management can be crucial for supporting fertility and emotional well-being. It is important to take time for healing, as with the right preparation and support, it is possible to find new hope and become pregnant again.
FAQ
What is the chance of getting pregnant after a miscarriage?
Many different factors influence the likelihood of getting pregnant after a miscarriage, including the woman's age and the causes of the miscarriage.
The chance of getting pregnant after a single miscarriage is usually very high, about 85%.
If recurrent miscarriages occur, the risk of another miscarriage increases. In general:
- After two miscarriages, the risk is about 20-30%.
- After three or more miscarriages, the risk rises to about 30-40%.
What is the risk of a miscarriage by pregnancy week?
The risk of a miscarriage strongly depends on the pregnancy week. In general, the risk significantly decreases as the pregnancy progresses.
Early Miscarriage
An early miscarriage occurs up to the 12th week of pregnancy and accounts for about 80% of all miscarriages. The causes are often genetic abnormalities, hormonal disorders, or immune factors.
In the first weeks (up to the 6th week), the risk is up to 50%, often before the pregnancy is even detected.
Between the 6th and 8th weeks, the risk is about 10-15%. After the 10th week, it drops below 5%.
Late Miscarriage
A late miscarriage occurs between the 13th and 24th week of pregnancy.
Between the 13th and 16th week, the risk is about 2-3%. After the 17th week, it drops further to below 1%.
After the 24th week, the survival rate for a premature birth with intensive medical care is relatively high.
How long does it take to get pregnant again after a miscarriage?
After a previous miscarriage, it is important to take time to recover both physically and emotionally. The time it takes to get pregnant again varies from woman to woman and depends on several factors:
After an early and uncomplicated miscarriage, the body can recover more quickly.
After a more advanced miscarriage or one with complications, such as a dilation and curettage (D&C), the recovery phase may take longer.
It is important for the hormonal balance to stabilize. This usually happens with the first menstrual period, which typically occurs 4 to 6 weeks after a miscarriage. After a D&C, it can take up to 8 weeks.
What are recurrent miscarriages?
Recurrent miscarriages (habitual abortions) generally refer to two or more consecutive pregnancies that end before the 20th week. Previously, it was thought to require three miscarriages, but even after two miscarriages, your gynecologist can initiate investigations.
When is the next ovulation after a miscarriage?
The timing of the next ovulation after a miscarriage can vary from woman to woman and depends on factors such as the average cycle length and the woman’s hormonal status.
Is a pregnancy after a miscarriage considered a high-risk pregnancy?
A pregnancy after a miscarriage is not automatically considered a high-risk pregnancy. A pregnancy can be classified as high risk due to the following factors: advanced maternal age, multiple pregnancies, pre-existing medical conditions, unhealthy lifestyle, etc.
What types of miscarriages are there?
-
Abortus completus (Complete Miscarriage): In this situation, the body has naturally completed the early pregnancy process by expelling all the tissue. The cervix then begins to close again.
-
Abortus imminens (Threatened Miscarriage): Signs of a miscarriage are present, but the pregnancy may still be continued. Symptoms may include vaginal bleeding and abdominal cramps.
-
Abortus incipiens (Beginning Miscarriage): Vaginal bleeding or rupture of membranes before the 20th week, with advanced cervical dilation.
-
Abortus incompletus (Incomplete Miscarriage): Opening of the cervix (cervix) and expulsion of the embryo and pregnancy tissue.
-
Anembryonic Pregnancy (Blighted Ovum): A non-viable pregnancy with a gestational sac but without a yolk sac or embryo visible on transvaginal ultrasound.
-
Molar Pregnancy (Hydatidiform Mole): A rare pregnancy complication in which abnormal tissue forms in the uterus. This results from a faulty interaction between maternal and paternal chromosomes at fertilization.
-
Habitual Abortion (Repeated Miscarriages): Three or more consecutive miscarriages before the 20th week of pregnancy. Causes can include genetic factors, hormonal imbalances, anatomical issues with the uterus, or autoimmune diseases.
-
Missed Abortion (Silent Miscarriage): The embryo or fetus dies in the uterus, but the body does not expel the tissue. This form of miscarriage is often detected only during an ultrasound.