Weibliche Unfruchtbarkeit
Laut Weltgesundheitsorganisation (WHO) liegt eine Unfruchtbarkeit, vor wenn ein Frau, innerhalb eines Jahres, trotz regelmäßigen, an ihren fruchtbaren Tagen ungeschützten Geschlechtsverkehrs nicht schwanger wird.
Ursachen weiblicher Unfruchtbarkeit
Endometriose
Bei Endometriose wächst Gebärmutterschleimhaut außerhalb der Gebärmutter. Mögliche Folgen sind Entzündungen und eingeschränkte Fruchtbarkeit. Etwa 5-10% aller Frauen leider unter Endometriose. Die Fruchtbarkeit ist nicht nur reduziert, sondern die Gefahr für Komplikationen während der Schwangerschaft und das Risiko einer Fehlgeburt sind erhöht.
Symptome: Bei vielen Frauen kann das abgelöste Gewebe der Ansiedelung („Endometriose-Herde“) unbemerkt und schmerzlos abfließen. Bei anderen Frauen führen die Gewebereste zu Entzündungen, Zysten und Verklebungen und können unterschiedlich starke Menstruationsschmerzen sowie Schmerzen im Bereich der Ansiedelung hervorrufen. Schmerzen werden oft krampfartig erlebt und können von Übelkeit, Erbrechen oder Durchfall begleitet sein.
Polyzystisches Ovarialsyndrom (PCO-Syndrom)
Das PCO-Syndrom ist eine der häufigsten hormonelle Erkrankungen von Frauen im gebärfähigen Alter. In Europa sind 5-10% der Frauen betroffen, oft ohne es zu wissen. Während der Name „viele Zysten“ suggeriert, liegen jedoch viele Eibläschen vor, die aufgrund fehlender Hormone nicht heranreifen können.
Bei PCO ist oft zu wenig FSH (follikelstimulierendes Hormon) und zu viel LH (luteinisierendes Hormon) vorhanden. Aufgrund des FSH Mangel reifen die Eibläschen nicht heran. Der Eisprung bleibt aus und es wird kein Progesteron (Gelbkörperhormon) produziert.
Zyklen bei Betroffenen sind meist sehr lange, Blutungen sind selten oder treten nie ein. 75% der Frauen mit PCO-Syndrom haben zusätzlich eine erhöhte Insulinresistenz.
Der erhöhte Insulinspiegel erforderlich für die Zuckeraufnahme führt zu einer Stimulation der Androgenproduktion in den Eierstöcken und in Folge zu einer erhöhten Konzentration männlicher Hormone (Androgene).
Symptome: Das PCO-Syndrom ist gekennzeichnet durch unregelmäßige oder ausbleibende Regelblutungen. Häufig kommt es zu keinem Eisprung. Auslöser kann auch ein leichtes Übergewicht und ein erhöhter Spiegel männlicher Hormone (Androgene) sein. Weitere Symptome sind Akne und vermehrte Körperbehaarung.
Verschlossene Eileiter
Die Eileiter verbinden den Eierstock mit der Gebärmutter. Sie sind entscheidend für die Befruchtung, da der Transport der Eizellen über den Eileiter erfolgt, wo sie in der Eileiterampulle von der Samenzelle befruchtet werden. Eilleiter können aber aufgrund von Entzündungen und Infektionen (häufig Chlamydien oder Gonorrhoe) oder auch Endometriose verklebt, verwachsen oder verschlossen sein.
Sind die Eileiter geschädigt oder komplett verschlossen, ist der Transport der Eizelle bzw. des Embryos erschwert oder unmöglich. Eine Prüfung der Eileiterdurchlässigkeit kann durch eine Bauchspiegelung oder eine spezielle Ultraschalluntersuchung erfolgen. Bei Eileiterverschluss wird häufig eine In Vitro-Fertilisation (IVF) empfohlen.
Hormonelle Störungen
Meist sind Hormonstörungen an einem veränderten Zyklus erkennbar. Blutungen bleiben ganz aus, kommen unregelmäßig oder es entstehen Zwischen- und Schmierblutungen. Schilddrüsenfunktionsstörungen sind oft Ursache für Unfruchtbarkeit. Die Schilddrüsenhormone beeinflussen den Zyklus, die weibliche Fruchtbarkeit und die Gehirnentwicklung des ungeborenen Kindes.
Schilddrüsenunterfunktion
Ursache: oft Hashimoto-Thyreoditits
Symptome: Müdigkeit, trockene Augen, Heiserkeit, Verstopfung oder Gewichtszunahme
Auswirkung auf weibliche Fruchtbarkeit: Zyklusstörungen, verlängerter Zyklus, seltene Blutung, bzw. Eisprung, Fehlgeburten
Schilddrüsenüberfunktion
Ursache: oft Morbus Basedow
Symptome: Bluthochdruck, Herzrhythmusstörungen, Nervosität, Gewichtsverlust, Durchfall, starkes Schwitzen, Schlafstörungen, Haarausfall, Erschöpfung, Stimmungsschwankungen
Auswirkung auf weibliche Fruchtbarkeit: Zyklusstörungen
Hyperprolaktinanämie (Erhöhung des Prolaktinspiegels)
Ursache: oft Schilddrüsenunterfunktion, Medikamente (Antidepressiva), Stress
Auswirkung auf weibliche Fruchtbarkeit: Zyklusstörungen, keine bzw. seltene Eizellreifung
Hyperandrogenanämie (Erhöhung der männlichen Hormone)
Mögliche Ursachen: PCO-Syndrom, Androgenitales Syndrom (Stoffwechselkrankheit), Tumor im Eierstock
Auswirkung auf weibliche Fruchtbarkeit: Fehlende Eizellreifung und ausbleibender Eisprung
Gelbkörperhormonmangel (Progesteronmangel)
Symptome: Schmierblutungen in der 2. Zyklushälfte, zu kurze 2. Zyklushälfte, Schlafstörungen
Auswirkung auf weibliche Fruchtbarkeit: Probleme bei der Einnistung des Embryos. Das Gelbkörperhormon (Progesteron) ist für die Einnistung der befruchteten Eizelle verantwortlich
Myome & Polypen
Myome sind häufig vorkommende, gutartige Knoten in der Gebärmutter. Knoten in der Gebärmutterhöhle oder in der Gebärmutterwand können die Einnistung eines Embryos erschweren. Je nach Größe können sie mittels einer minimalinvasiven Operation entfernt werden.
Polypen sind gutartige und meist harmlose Wucherungen der Gebärmutterschleimhaut. Häufig gehen sie mit der nächsten Monatsblutung ab. Ein ungünstig gelegener Polyp kann sich jedoch auf die Fruchtbarkeit auswirken. Ein Polyp kann mittels einer Ausschabung (Kürettage) entfernt werden.
Symptome: Häufig werden Myome oder Polypen gar nicht bemerkt.
Fehlbildung der Gebärmutter
Die Gebärmutter ist ein umgekehrtes birnenförmiges Muskelorgan, eine glatte Höhle, die mit Schleimhaut ausgekleidet ist, in der ein Embryo heranwachsen kann. Jede Fehlbildung der Gebärmutter kann Einfluss auf die Fruchtbarkeit haben. Es gibt verschiedene Arten von Fehlbildungen:
Uterus arcuatus: Die herzförmige Gebärmutter ist die mildeste Art der Fehlbildung. Dabei weist der obere Teil der Gebärmutter eine kleine Einbuchtung auf, der die Gebärmutter herzförmig erscheinen lässt. Sie scheint keinen Einfluss auf die weibliche Fruchtbarkeit oder die Einnistung zu haben.
Uterus septus: Eine Trennwand in unterschiedlicher Länge und Dicke befindet sich in der Gebärmutter. Dies kann die Fruchtbarkeit einschränken und Fehlgeburten begünstigen.
Fehlbildungen können operativ behandelt werden, so dass eine natürliche Schwangerschaft möglich ist.
Frühzeitige Wechseljahre
Die vorzeitige Menopause ist das dauerhafte Ende der Menstruationsperiode vor dem 40. Lebensjahr. Sie tritt ein, wenn die Eierstöcke nicht mehr regelmäßig Eizellen freisetzen und der Eisprung ausbleibt. Die vorzeitigen Wechseljahre gehen mit einer Hormonumstellung des weiblichen Körpers einher.
Symptome: Während einige Frauen keine Symptome wahrnehmen, leiden andere Frauen an den üblichen Symptomen der Menopause: Hitzewallungen, Stimmungsschwankungen und Nachtschweiß.
Mögliche Ursachen: Genetische Fehlbildungen, Autoimmunerkrankungen, Viruserkrankungen, operative Entfernung der Eierstöcke und Gebärmutter, Chemo- bzw. Strahlentherapie, Toxine wie Tabak.
Störungen des Immunsystems
Der Grund für weibliche Infertilität kann auch in einer gestörten Immunreaktion des weiblichen Körpers liegen. Das eigene Immunsystem identifiziert den Embryo als Fremdkörper, die es als Eindringling bekämpft.
Diagnose der weiblichen Unfruchtbarkeit
Die Diagnose der Ursache für unerfüllten Kinderwunsch ist entscheidend um die richtige Therapieform zu wählen.
Anamnese - Gesundheitsgeschichte
Wichtig ist das Abklären der persönlichen Gesundheitsakte, inkl. Regelmäßigkeit des Zyklus, möglicher gynäkologischer Vorerkrankungen, Operationen und Medikamente.
Gynäkologische Untersuchung
Im Rahmen einer gynäkologischen Untersuchung können bereits erste Anzeichen auf Endometriose, Myome und Eierstockzysten identifiziert werden.
Ultraschalluntersuchung
Mittels Ultraschalluntersuchung können wichtige Funktionen der Gebärmutter untersucht werden. Der Aufbau, die Lage und Größe der Gebärmutter, sowie mögliche Erkrankungen wie Myome, Polypen oder Eierstockzysten können diagnostiziert werden. Eine Ultraschalluntersuchung ist auch relevant, um die Reifung der Eibläschen und der Gebärmutterschleimhaut, bzw. das Ausbleiben des Zyklus zu verfolgen.
Hormonstatus
Da Hormonstörungen häufig Ursache für unerfüllten Kinderwunsch sind, ist es ratsam den Hormonspiegel zu testen. Der Hormonstatus sowie die Änderungen während des Zyklus geben Aufschluss über die weibliche Fruchtbarkeit. Auch die Eizellreserve wird mittels Hormonwerten bestimmt. Zwischen dem zweiten und fünften Zyklustag sind folgende Werte entscheidend: FSH, LH, TSH, Östrogene, Prolaktin, und Androgene. In der zweiten Zyklushälfte können Progesteron und Östrogenwerte aussagekräftig sein.
Eileiteruntersuchung mittels HyCoSy
Mittels Ultraschalltechnik (Hysterokontrastsonographie „HyCoSy“), kann die Durchgängigkeit der Eileiter weitgehend schmerzfrei geprüft werden. Bei einer HyCoSy wird echoreicher Schaum mittels eines dünnen Katheders in den Gebärmutterhöhle gespült. Die Durchgängigkeit der Eileiter kann so auf beiden Seiten überprüft und via Ultraschallmonitor mitverfolgt werden. Die Vorteile der HyCoSy liegen in der geringeren Strahlenbelastung gegenüber dem früher häufig durchgeführten Eileiterröngten (HSG). Im Gegensatz zur operativen Bauchspiegelung ist Eileiteruntersuchung mittels HyCoSy nicht invasiv.
Bauchspiegelung
Bei Verdacht auf Verwachsungen, Verklebungen oder auf Endometriose, kann die Diagnostik mittels Bauchspiegelung (Laparoskopie) erfolgen. Unter Narkose wird durch einen kleinen Bauschnitt ein Laparoskop, ein röhrenförmiges Instrument in die Bauchhöhle eingeführt. Das Instrument führt zu einem genauen Bild der inneren Fortpflanzungsorgane, das via externem Monitor angezeigt werden kann.
Gebärmutterschleimhaut-Biopsie (bei Einnistungsversagen)
Eine Untersuchung der Gebärmutterschleimhaut kann Aufschluss über natürliche "Killerzellen" (NK-Zellen) und Plasmazellen geben. Bei der Endometriumbiopsie werden mittels Katheder kleine Gewebstücke der Gebärmutterschleimhaut entnommen und mikroskopisch analysiert.
Gebärmutterspiegelung
Bei Verdacht auf Fehlbildungen der Gebärmutter oder Schleimhautveränderungen kann mittels einer Gebärmutterspiegelung eine weiterführende Diagnostik sowie gleichzeitig bereits die Therapie durchgeführt werden.
Der Weg zum Wunschkind
Die Ursache der Infertilität ist entscheidend für die Behandlungsoption. Zu den Behandlungsmethoden zählen Zyklusmonitoring, hormonelle Stimulation, Insemination, In-Vitro-Fertilisation und ICSI.
Zyklusmonitoring
Die sanfteste Methode, um schwanger zu werden liegt im Zyklusmonitoring. Da die fruchtbaren Tage nahe am Eisprung sind, ist es entscheidend diese zu kennen. Zyklusmonitoring kann bei einem regelmäßigen Zyklus alleine durchgeführt werden, häufig unterstützen Kinderwunschzentren mittels Ultraschall- und Hormondiagnostik. Somit kann die Reifung des Eibläschens überwacht und der Eisprung vorausgesagt werden. Kurz vor dem Eisprung wird Geschlechtsverkehr empfohlen. Eine Schwangerschaft kann hiermit auf natürlichem Wege erfolgen.
Hormonelle Stimulation
Im ersten Schritt wird der weibliche Zyklus beobachtet. Wichtig ist die Frage, ob ein Eisprung stattfindet. Ist dies nicht der Fall, so hat dies oft hormonelle Ursachen, wie etwa das PCO-Syndrom, eine Schilddrüsenfunktionsstörung, vermehrt männliche Hormone oder auch ein erhöhter Prolaktinwert. Die Eierstöcke können mittels Hormonbehandlung stimuliert werden, der Zyklus kann sich dadurch normalisieren. Ist ein regelmäßiger Zyklus wiederhergestellt, so kann ein Kind auf natürlichem Weg zu Hause empfangen werden.
Intrauterine Insemination
Die Insemination ist ein schonendes Verfahren, bei dem männliche Spermien direkt in die Gebärmutter gespült werden. Spermien wird hierdurch eine Befruchtung erleichtert, sie sind näher zur Eizelle. Diese Methode kann mit oder auch ohne Hormonstimulation durchgeführt werden. Es ist kein operativer Eingriff erforderlich.
In-Vitro-Fertilisation (IVF) & ICSI
Bei einer In-Vitro-Befruchtung erfolgt die Befruchtung außerhalb des Körpers im Reagenzglas. Eizellen werden mit Spermien in einer Petrischale zusammengebracht und erleichtern somit eine Befruchtung.
Die ICSI-Behandlung ist eine spezielle Form der IVF-Behandlung, bei der das beste Spermium unter einem Mikroskop ausgewählt und vorsichtig in die Eizelle injiziert wird. Die ICSI-Methode ist erforderlich, wenn die Spermienqualität stark eingeschränkt ist.

BOOST YOUR EGGS Unterstütze Deine Fruchtbarkeit
All diese Behandlungsoptionen erfordern eine gezielte Zufuhr der relevanten Nährstoffe zur Verbesserung der Fruchtbarkeit und Vorbereitung des weiblichen Körpers auf eine Schwangerschaft.
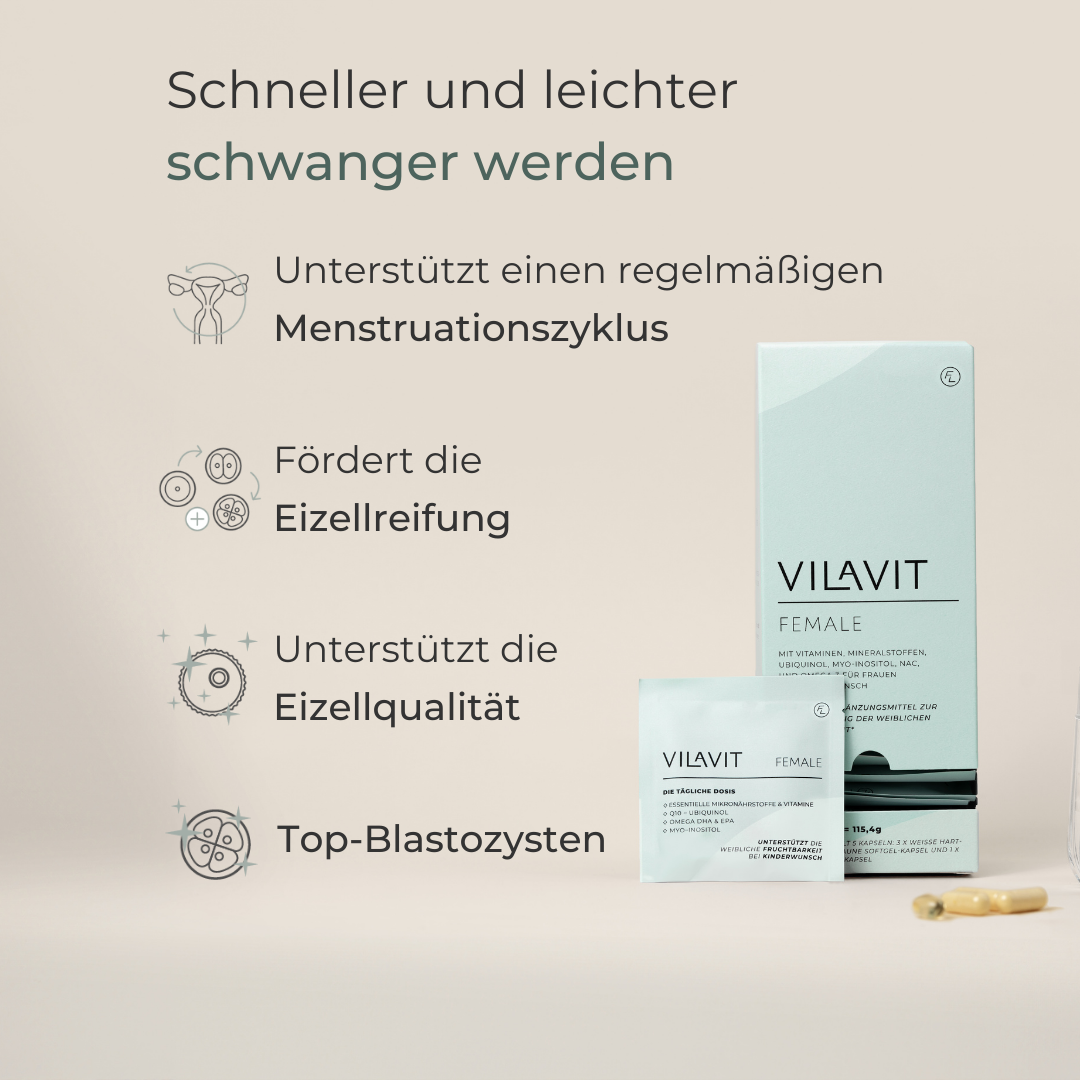
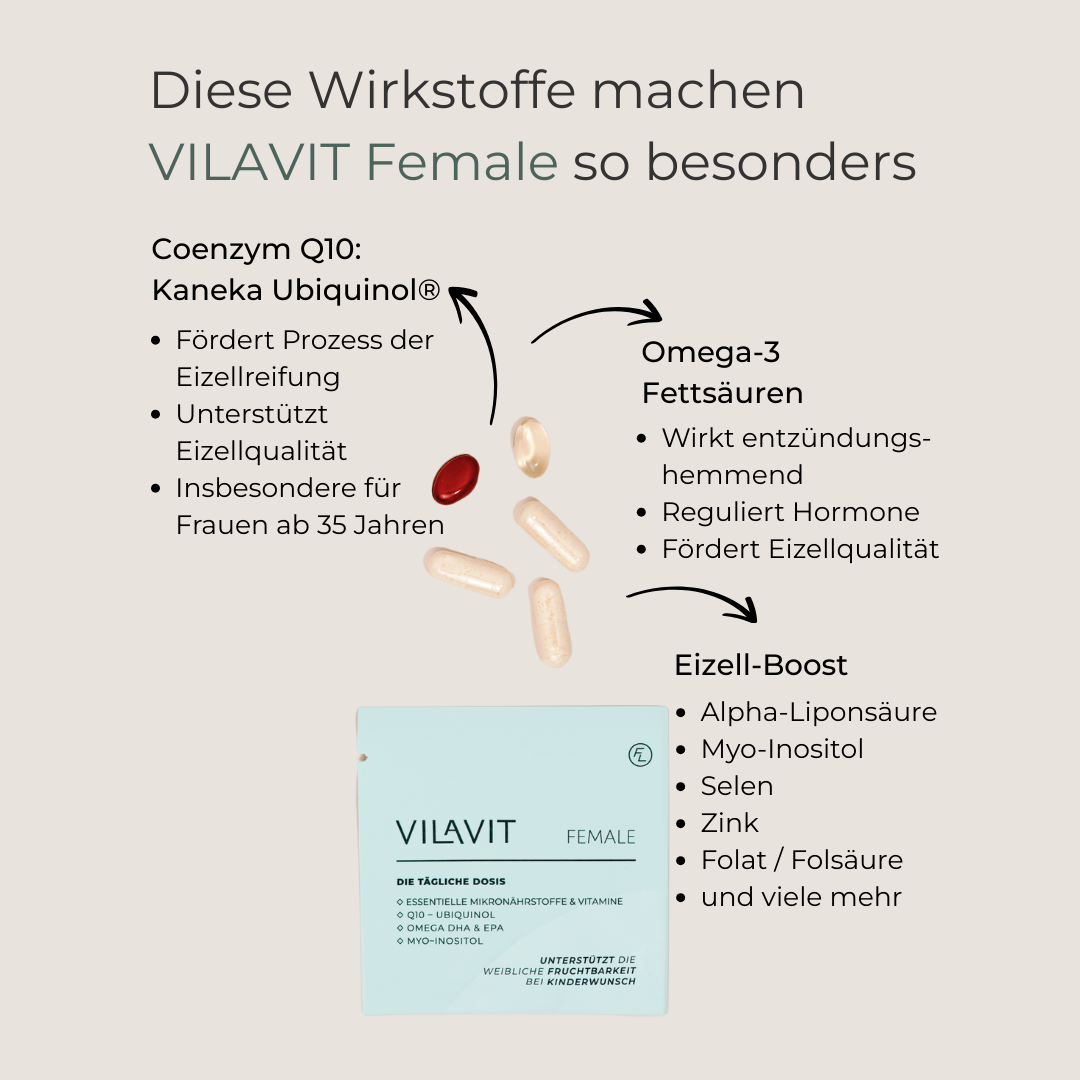
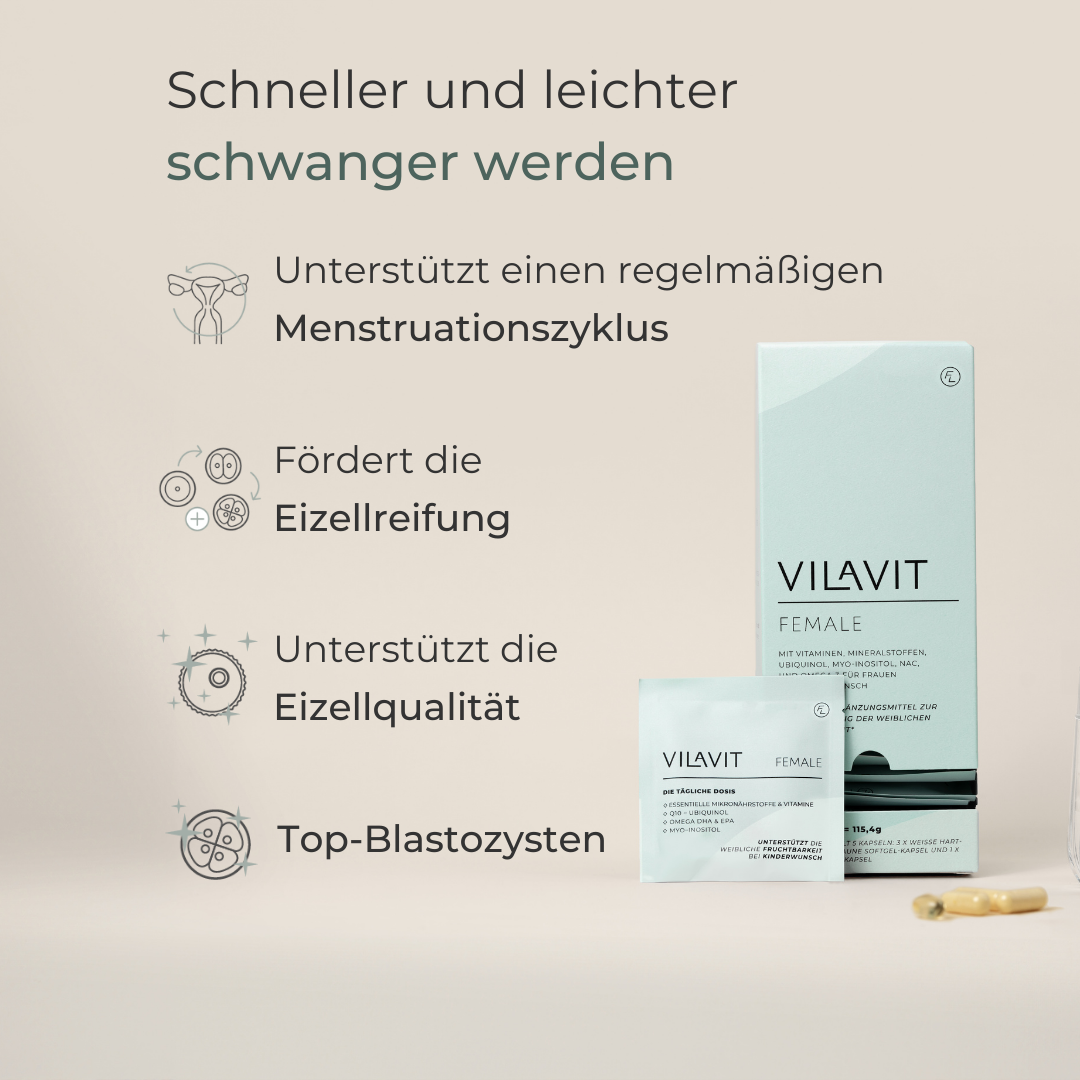
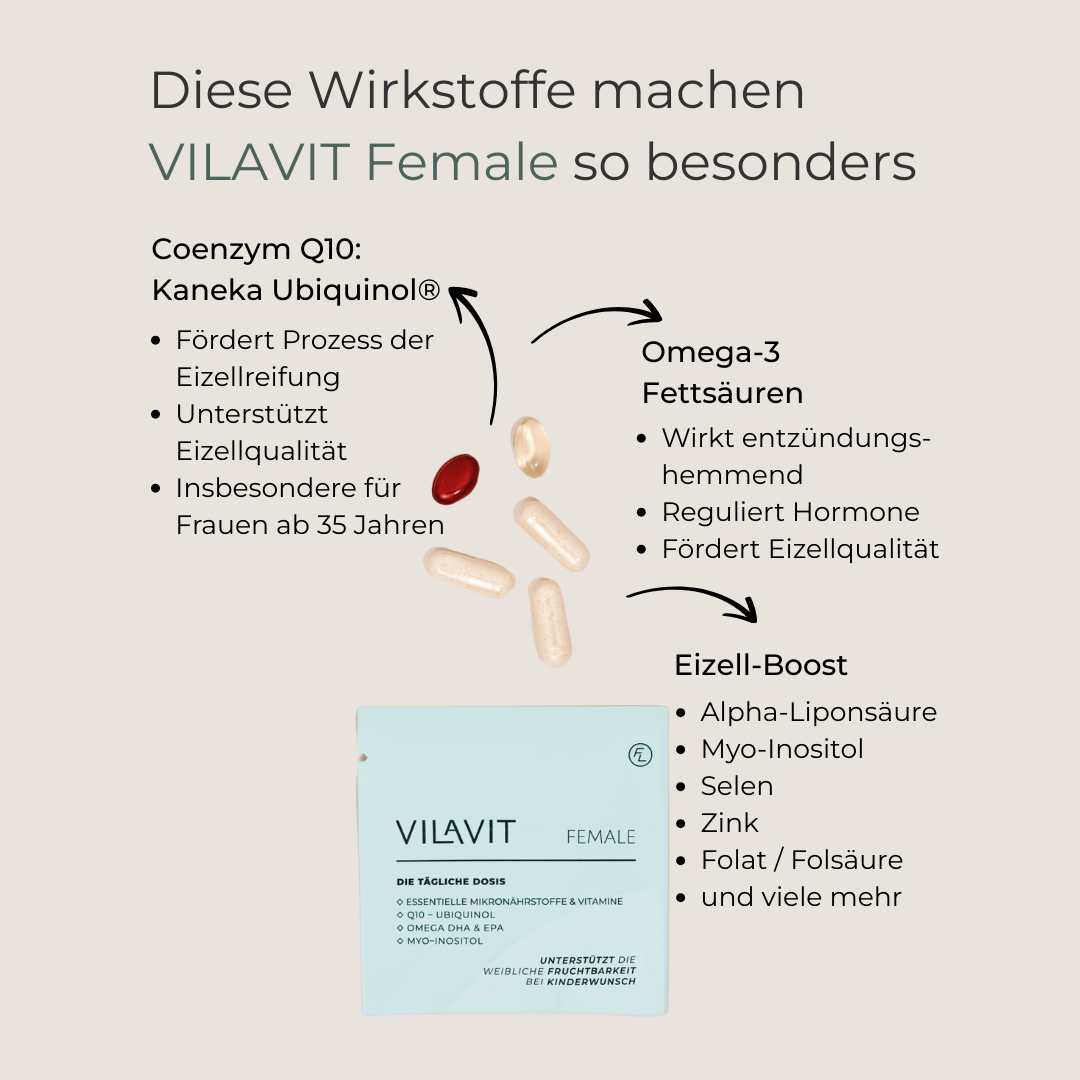
VILAVIT Female unterstützt die Eizellreifung und -qualität, sowie in Folge die Embryoqualität. Auch bei der Wiederherstellung eines regelmäßigen Zyklus mit Eisprung kann VILAVIT unterstützten.
Die VILAVIT Produktreihe wurde von unserem Expertenteam entwickelt und enthält alle relevanten Mikronährstoffe zur optimalen Unterstützung der Eizellqualität & Embryoqualität.
VILAVIT Female
- Regular price
-
€69,00 - Regular price
-
- Sale price
-
€69,00
Share






Die andere Hälfte der Gleichung
In rund 40% der Fällen liegt die Ursache des unerfüllten Kinderwunsches beim Mann.
Auch die Spermienqualität kann unterstützt werden.