Everything you need to know at a glance:
-
Oligozoospermia occurs when the sperm concentration in the ejaculate is below 16 million/ml.
-
The sperm concentration is not always constant, but can change within weeks due to stress, illness or environmental factors.
-
A spermiogram after 3-5 days of abstinence is required to assess the number, motility and morphology of the sperm.
-
A healthy lifestyle with a balanced diet, exercise, abstinence from smoking and alcohol promotes sperm quality.
-
Studies show that coenzyme Q10 and omega-3 fatty acids can actually measurably improve sperm quality.
Getting pregnant despite oligozoospermia - here's how
If the long-awaited pregnancy fails to materialize, one of the most common causes of male infertility can be oligozoospermia, also known as oligospermia. The number of sperm is greatly reduced compared to the ejaculate of a fertile man. A low sperm count can negatively affect the chances of natural conception, as the low number of sperm is less likely to move up through the female reproductive tract into the uterus and fallopian tubes to fertilize the egg. The desire to have children often remains unfulfilled.
How is oligozoospermia defined?
According to the World Health Organization (WHO), oligozoospermia is diagnosed when the concentration of sperm in a man's ejaculate is less than 16 million sperm per milliliter.
In addition, the WHO establishes size classifications for severe oligozoospermia - approximately less than 5 million sperm/ml, often combined with low motility and abnormal morphology (oligoasthenoteratozoospermia).
The analysis of sperm is performed by a semen analysis in the andrology laboratory, for which a semen sample (after no more than 3-5 days of abstinence) is required. The number of sperm present is examined under the microscope. The degree of oligozoospermia can be classified as moderate, mild or severe.
What are the causes of oligozoospermia?
Hormonal imbalances
Sperm production is largely regulated by hormonal signals. A hormonal imbalance can affect the production and quality of sperm. The relevant hormones include
- Testosterone: A low testosterone level can inhibit spermatogenesis (sperm maturation/production)
- FSH (follicle stimulating hormone) and LH (luteinizing hormone):These hormones are responsible for regulating the production of sperm and testosterone in the testicles.
Diseases such as Klinefelter's syndrome or hypogonadism can lead to hormonal imbalances and thus cause oligozoospermia.
Genetic diseases
Genetic abnormalities play a significant role in the development of oligozoospermia. The most common genetic causes include
- Klinefelter syndrome: a chromosomal abnormality in which men have an extra X chromosome, resulting in reduced sperm production.
- Y chromosome microdeletion: Small losses on the Y chromosome can significantly affect sperm production.
Environmental and lifestyle factors
Certain environmental and lifestyle factors can have a negative impact on sperm count:
- Smoking: Nicotine and other harmful substances in tobacco smoke can reduce sperm quality and count.
- Alcohol consumption: Excessive alcohol consumption can lead to hormonal disorders and reduced sperm production.
- Drug abuse: The use of drugs such as cannabis or steroids can impair sperm production.
- Overweight and obesity: Excessive body fat can cause hormonal imbalances that interfere with sperm production.
Urogenital diseases
Certain infections and inflammatory diseases of the male reproductive organs - especially the testicles, epididymis or vas deferens - can impair sperm production or sperm transport.
- Testicular inflammation (orchitis):Infections, such as mumps, can inflame the testicles and lead to permanent damage to the testicular tissue, which can impair sperm production.
- Epididymitis: Inflammation of the epididymis can affect sperm storage and maturation.
Anatomical problems
Anatomical abnormalities can also affect sperm production:
- Varicocele: An enlarged vein in the scrotum can interfere with blood circulation to the testicles and affect sperm production.
- Congenital anomalies: Congenital malformations of the reproductive organs can interfere with sperm production or sperm transportation.
Exposure to toxins
Long-term exposure to chemical substances or environmental toxins can reduce sperm count. Examples include:
- Heavy metals: lead, mercury and other metals can affect sperm quality.
- Industrial chemicals: Exposure to certain chemicals in industry can also have a negative impact on sperm production
Can you get pregnant despite oligospermia?
The good news: Yes, it is possible to get pregnant with oligozoospermia. However, the chances of a spontaneous pregnancy are greatly reduced, so it is strongly recommended that you consult a specialist. For a targeted therapy, it is important to get to the bottom of the cause of oligozoospermia.
The classification of oligozoospermia according to the severity of the sperm count is crucial for the assessment of fertility and the choice of treatment options. As a rule, the lower the sperm concentration, the greater the impairment of fertility. The WHO defines the following categories:
|
Severity |
Sperm concentration in the ejaculate |
Explanation |
|
Mild oligozoospermia |
10-16 million/ml |
Slightly below the WHO limit; spontaneous pregnancy is still possible. |
|
Moderate oligozoospermia |
5-10 million/mll |
Fertility significantly reduced; often limited motility. |
|
Severe oligozoospermia |
< 5 million/ml |
Severely restricted fertility; usually also poor motility and morphology. |
Treatment of oligospermia
The following ways can help to get pregnant despite oligozoospermia.
Correcting the underlying causes
Drug treatment: If there are hormonal imbalances or other treatable causes of oligozoospermia, medication or hormone replacement therapy can help to improve sperm production.
Treatment of infections: Bacterial or viral infections of the testicles, epididymis or prostate are usually treated with antibiotics. It is important to recognize the infection early and cure it completely - also to avoid permanent damage to the vas deferens or testicular tissue.
Surgical interventions: In the case of anatomical problems such as a varicocele (dilated veins in the scrotum), surgery may be considered to improve blood circulation in the testicles and promote sperm production
Healthy lifestyle
An active lifestyle with plenty of exercise and a balanced diet, abstaining from alcohol and nicotine is recommended for healthy sperm production.
Micronutrients
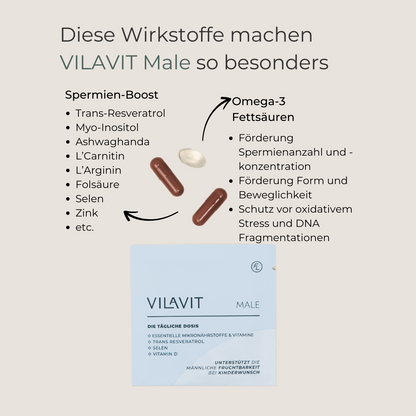
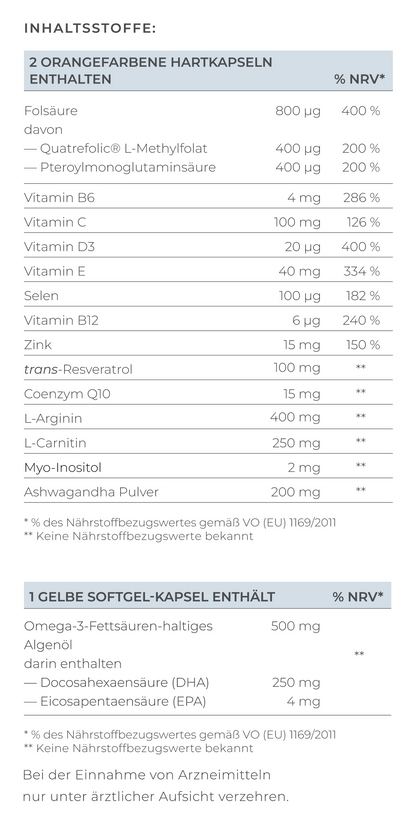
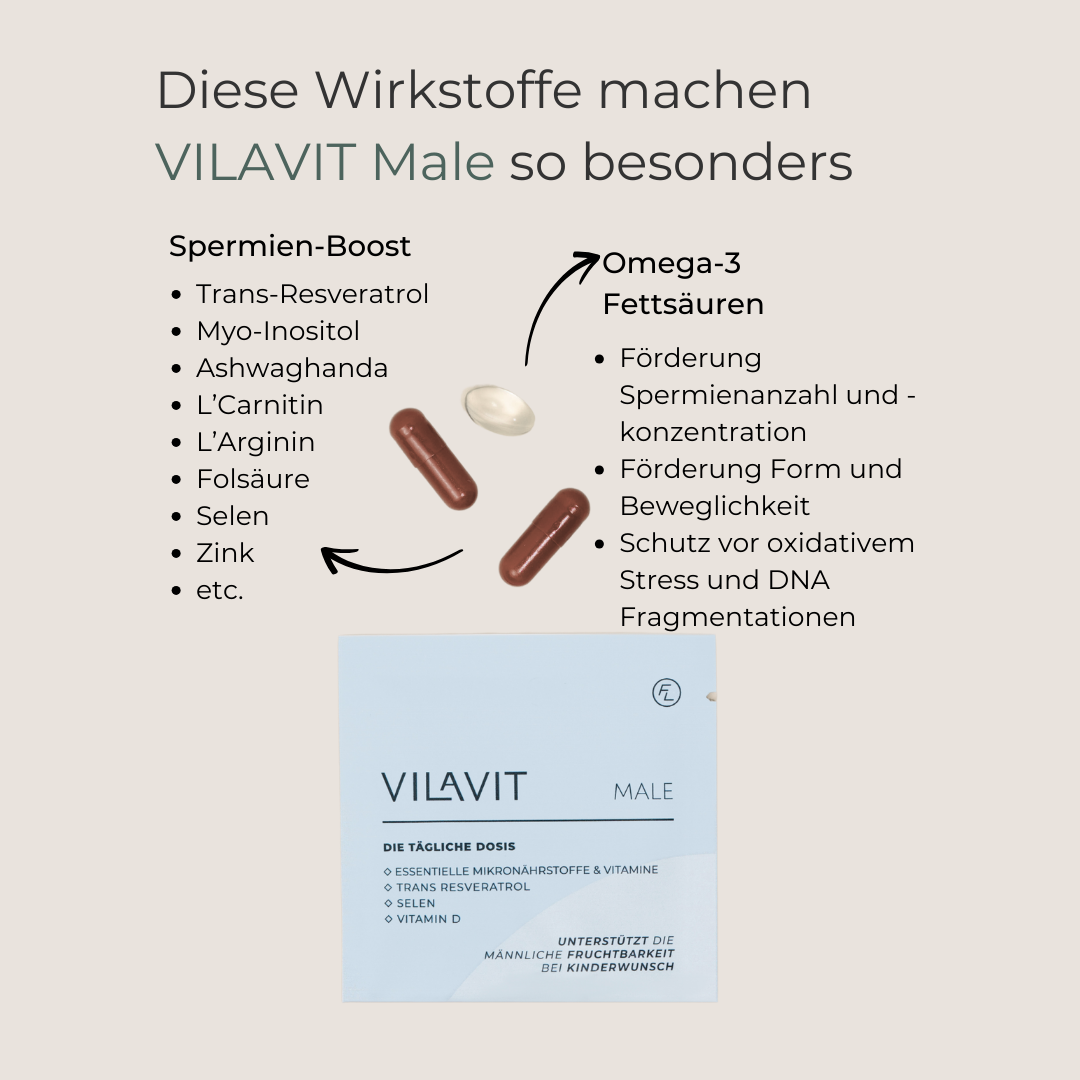
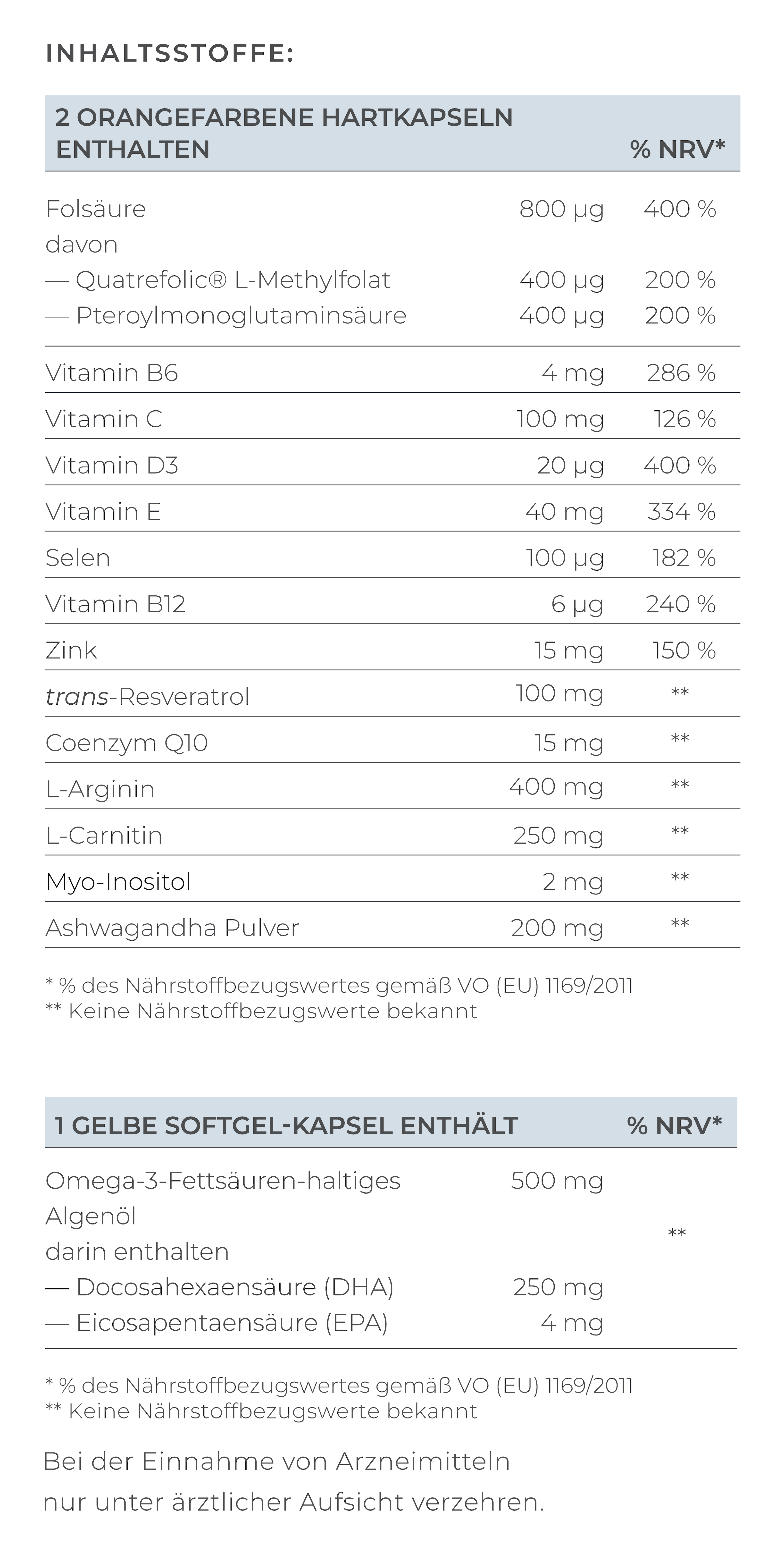
Scientific studies have identified positive effects of certain active ingredients on the total sperm count. The most important nutrients include
Clinical studies with certain micronutrients have also shown an improvement in sperm shape, sperm motility and a reduction in DNA fragmentation. These include:
Micronutrients in their bioavailable form, optimally dosed (based on scientific results), are crucial for an effective effect. VILAVIT Male contains all the relevant active ingredients to promote sperm count and sperm quality. Developed by leading reproductive physicians.
Insemination (IUI)
In cases of mild oligozoospermia, insemination (IUI) can be a cost-effective and simple option. The prerequisite is the collection of 2-3 million progressively motile sperm (after semen preparation).
In vitro fertilization (IVF) or ICSI
In cases of moderate or severe oligozoospermia, in vitro fertilization or ICSI may be necessary. In ICSI, a single living sperm is selected using state-of-the-art technology and injected into the egg to fertilize it.
Conclusion
Even though oligozoospermia can reduce the chances of a natural pregnancy, there are numerous ways and treatment options to increase the chances of successful conception. Medical support from specialists, lifestyle changes if necessary and micronutrients are the key to a successful pregnancy despite a low concentration of sperm.
Sources
- Safarinejad M.R. Efficacy of Coenzyme Q10 on Semen Parameters, Sperm Function and Reproductive Hormones in Infertile Men.Urol.2009
- Agarwal A, Prabakaran SA, Allamaneni SS. What an andrologist/urologist should know about free radicals and why. 2006
- Hosseini B, Nourmohamadi M, Hajipour S, Taghizadeh M, Asemi Z, Keshavarz SA, Jafarnejad S. The Effect of Omega-3 Fatty Acids, EPA, and/or DHA on Male Infertility: A Systematic Review and Meta-analysis. J Diet Suppl. 2019
- Jannatifar R, Parivar K, Roodbari NH, Nasr-Esfahani MH. Effects of N-acetyl-cysteine supplementation on sperm quality, chromatin integrity and level of oxidative stress in infertile men. Reprod Biol Endocrinol. 2019
- Mongioì LM, Perelli S, Condorelli RA, Barbagallo F, Crafa A, Cannarella R, La Vignera S, Calogero AE. The Role of Resveratrol in Human Male Fertility. Molecules. 2021