In the world of the desire to have children, there are not only ways to increase women's fertility - on the contrary: testicular sperm extraction (TESE), sometimes also called testicular biopsy, offers men whose sperm contains too few or no sperm cells a way to still obtain enough sperm to enable fertilization. This means that couples with azoospermia or cryptospermia do not have to give up their desire to have children!
The most important facts about testicular sperm extraction (TESE):
-
Testicular sperm extraction is a way for men with little or no sperm to conceive a child
-
Common indications for TESE are azoospermia (no sperm in the ejaculate), crytozoospermia (extremely low sperm count in the ejaculate) and genetic or hormonal disorders (such as Klinefelter's syndrome, which impairs sperm production)
-
TESE is a surgical procedure that can be performed under local or general anesthesia
-
TESE is almost always combined with ICSI to perform fertilization, as fertilization is likely even with limited sperm quality and quantity
-
TESE is also called testicular biopsy
What is TESE?
TESE stands for testicular sperm extraction and is sometimes also called testicular biopsy. The procedure is usually used when a man has too little or no sperm in his semen. A needle connected to a syringe is inserted into the testicles. A vacuum is then created, and the tip of the needle is moved in the testicle to break through the seminiferous tubules and extract sperm from different areas of the testicle. Sometimes several incisions are also used to obtain sperm from different areas of the testicle.
In micro-TESE, a subtype of TESE, a surgical microscope is used to collect material from the seminiferous tubules most likely to contain sperm (Esteves S. C., 2022). However, this requires a cross-section through the testicle instead of a syringe.
Unfortunately, there is no guarantee of success for TESE, as it is not possible to determine in advance how many sperm are present in the testicles. Nevertheless, many men have already achieved great results.
How does TESE work?
Before a TESE, a detailed medical history, information and several examinations are always carried out to determine the need for a TESE and to prepare the patient in the best possible way. TESE is performed either under local or general anesthesia (Flannigan, R., et al., 2017). Sometimes hormonal treatment before the procedure can also be useful.
Is TESE suitable for me?
TESE is performed in cases of obstructive azoospermia, among others. In this case, sperm production is intact, but no sperm reach the ejaculate (semen) due to a blockage in the vas deferens. In the case of obstructive azoospermia, there is usually a good chance of successful TESE. In men with non-obstructive azoospermia, there is also a chance that sperm will be present in the testicles, but it is much more difficult to make an assessment before the procedure.
What happens after the procedure?
After the procedure, the sperm are removed from the tissue and then, if enough sperm can be obtained, ICSI can be performed. In this procedure, a sperm is injected into an egg before the embryo is subsequently implanted into the woman's uterus
What is the chance of success?
There is a great deal of disagreement in the studies as to how successful TESE is. However, most men who undergo TESE would hardly have any other chance, which is why even minor successes can be very significant for those affected.
However, it can be deduced from the data that with ICSI, the fertilization rate after micro-TESE is 57% on average. Unfortunately, there is still very little data available regarding miscarriages and live births. However, the available studies indicate that around 24% of couples in which the sperm was obtained by micro-TESE had a live birth (Esteves S. C., 2022).
What are the risks?
TESE is a surgery and therefore has similar complications to other surgeries. The most common complication of TESE is bruising or swelling of the testicles. Overall, side effects are rare with TESE, but more serious complications are of course also possible (Esteves S. C., 2022). However, the doctor treating you will inform you before the procedure. It is therefore best if you ask them your concerns and questions about your individual situation, as the risks must be weighed up individually depending on the procedure, previous illnesses or medication.
Frequently asked questions about TESE:
Is TESE painful?
TESE is a surgical procedure. Patients do not feel any pain during the procedure itself, but pain is possible afterwards. However, this usually subsides relatively quickly and without complications.
Is there anything else I can do to improve my sperm quality and perhaps even avoid TESE?
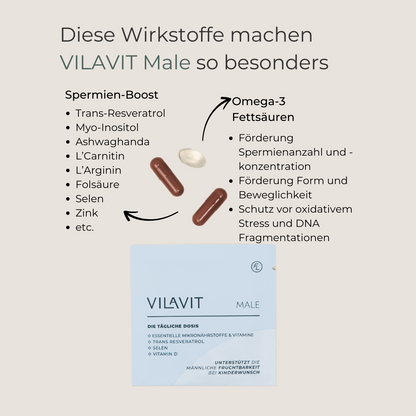
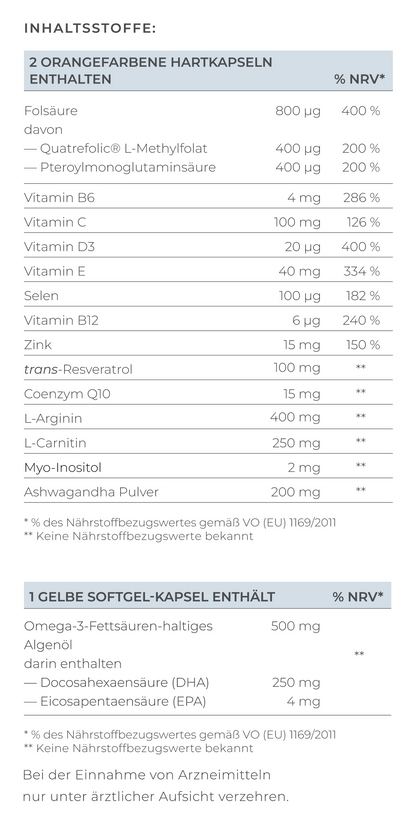
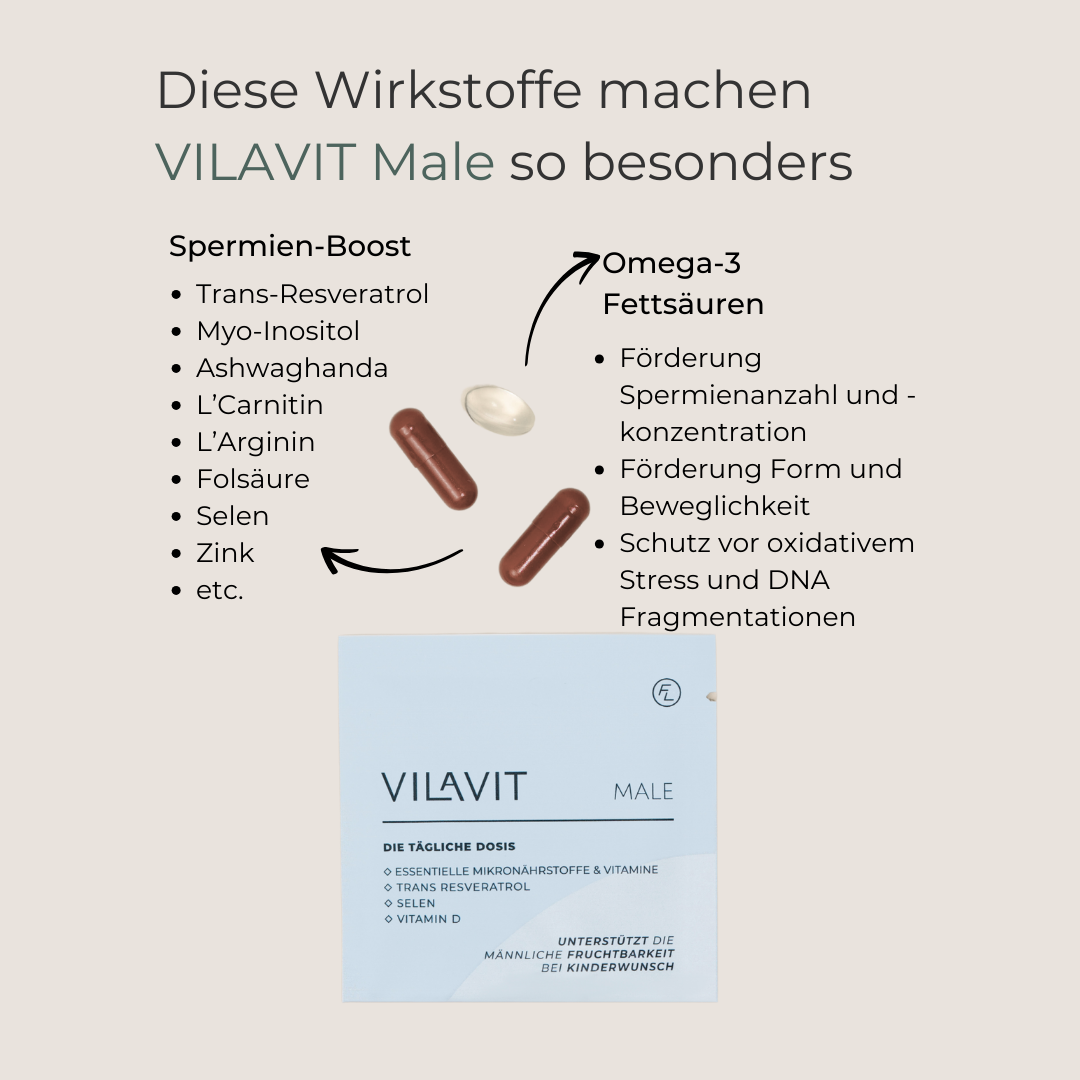
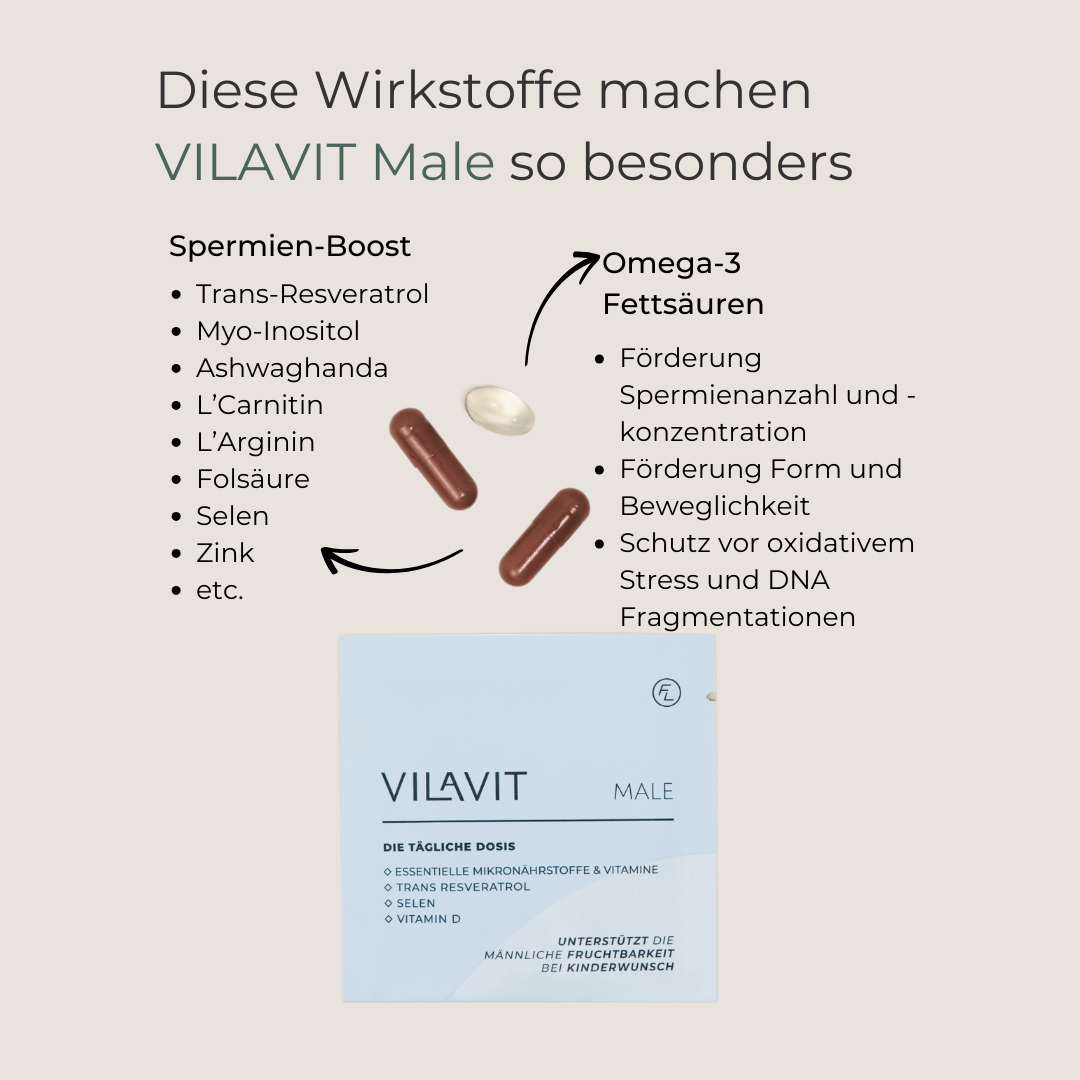
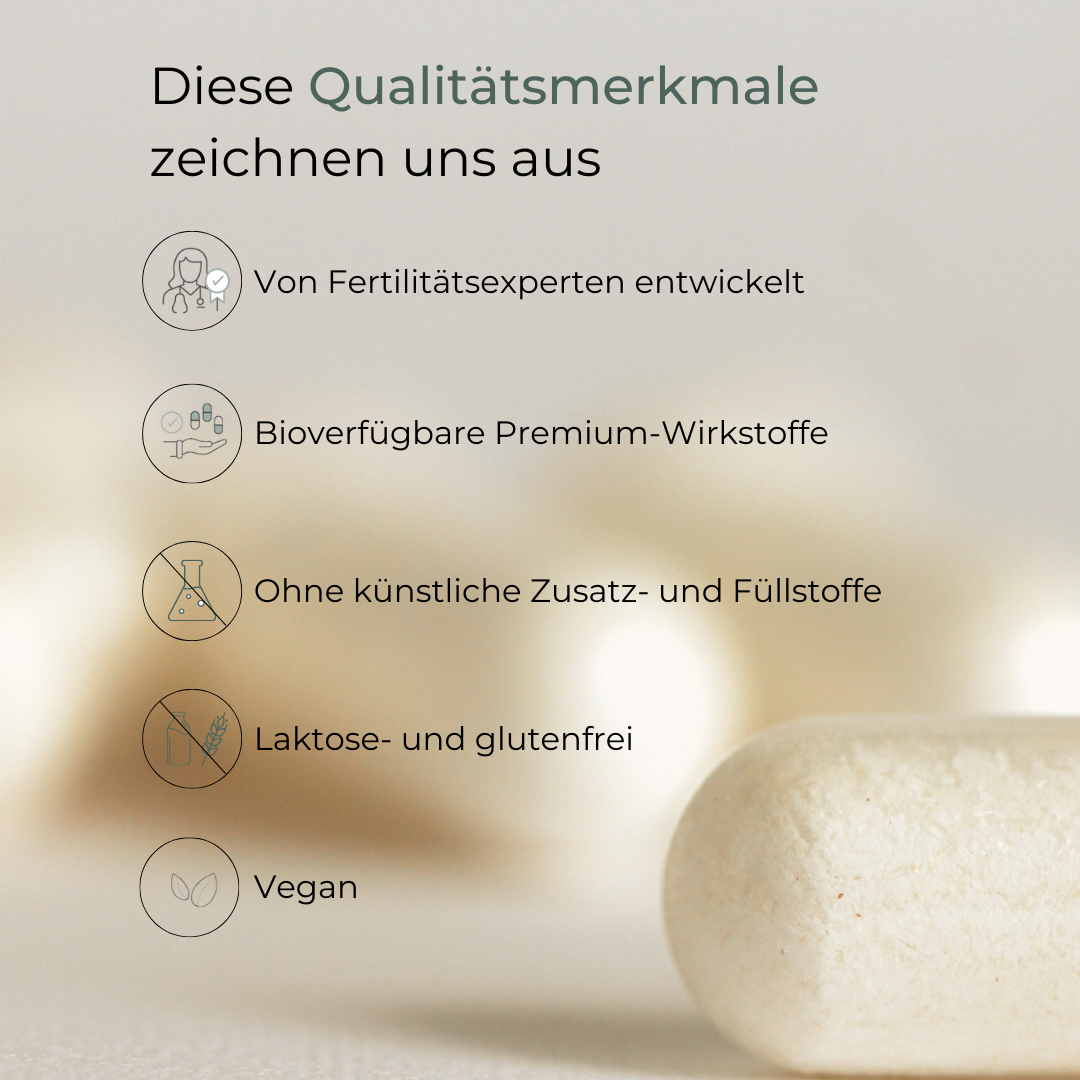
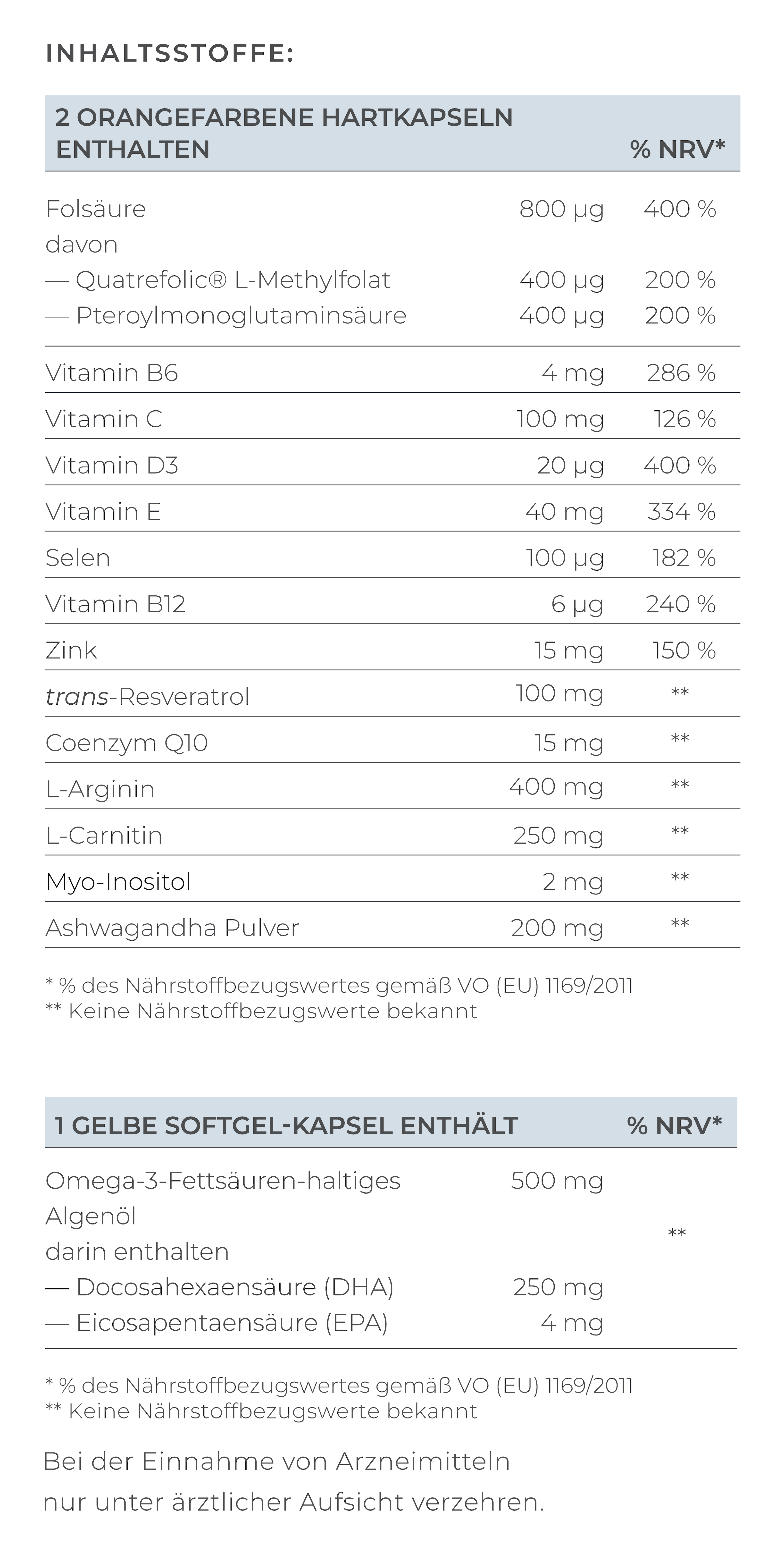
Yes, of course! Many lifestyle factors can contribute to improving sperm quality. Otherwise, high-quality micronutrient supplements such as VILAVIT Male, which has been specially developed to improve sperm quality, can make an important contribution.
Where can I have a TESE performed?
TESE is often offered by fertility centers or clinics. Some doctors (in private practice) also offer TESE. The surgery is then usually performed in a day clinic. Some public hospitals also have departments where fertility treatments can be carried out.
References:
- Esteves S. C. (2022). Microdissection TESE versus conventional TESE for men with nonobstructive azoospermia undergoing sperm retrieval. International braz j urol : official journal of the Brazilian Society of Urology, 48(3), 569–578.
- Flannigan, R., Bach, P. V., & Schlegel, P. N. (2017). Microdissection testicular sperm extraction. Translational andrology and urology, 6(4), 745–752.