Key Facts at a Glance
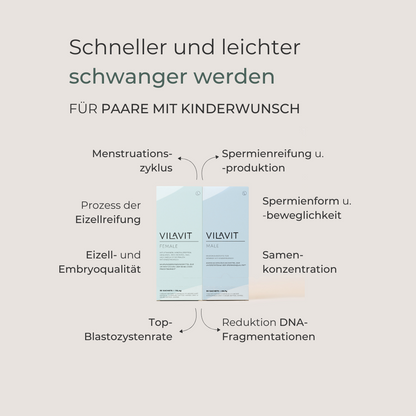
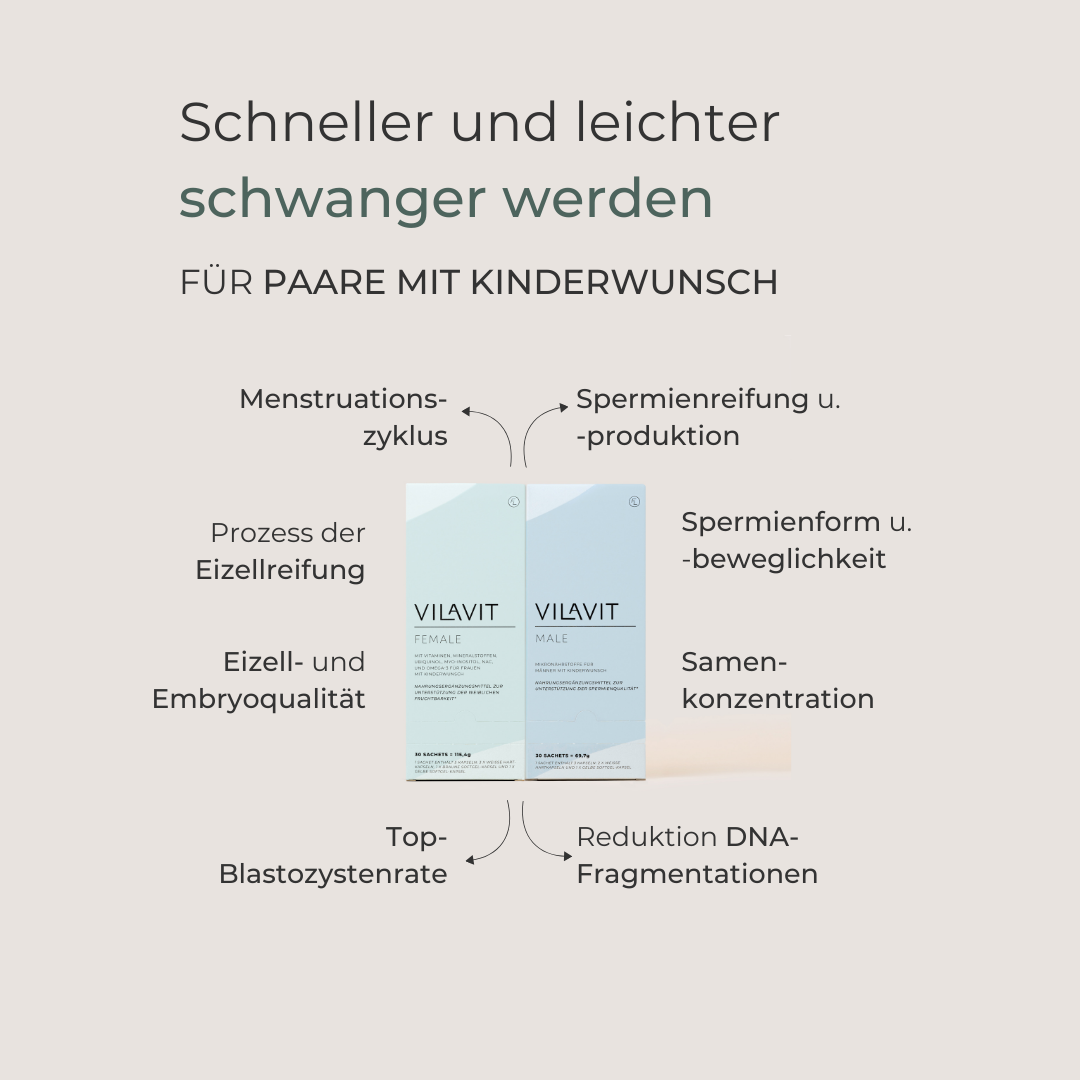
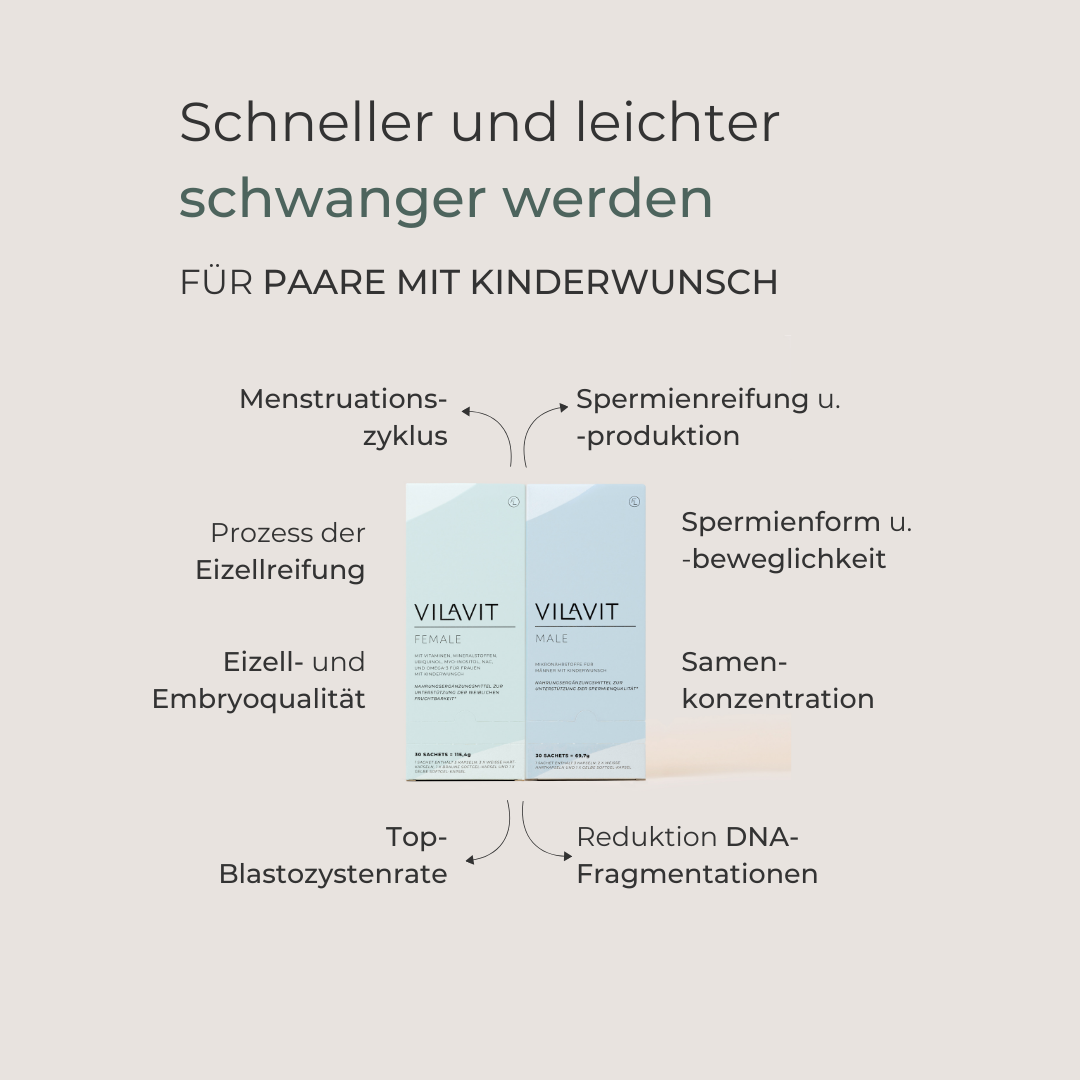
- Egg and sperm quality are crucial for fertilization and implantation.
- A woman’s age strongly affects egg quality.
- Quality declines from the mid-30s, and chromosomal risks increase after 40.
- Healthy nutrition, exercise, sleep, stress reduction, avoiding smoking/alcohol, and targeted micronutrients can help.
- In the lab, embryos are fertilized via IVF or ICSI and cultured in incubators.
- Embryo quality is assessed by cell division, symmetry, and fragmentation.
- Blastocysts and time-lapse monitoring help select the embryo with the highest implantation potential
From an embryological perspective, how important do you consider egg and sperm quality to be for the success of fertility treatment?
Nenad Nikolić: Egg and sperm quality are crucial. Good egg quality influences both fertilization and early embryonic development. Sperm quality is particularly important for successful fertilization and the stability of genetic material.
What role does a woman's biological age play in relation to egg quality?
Nenad Nikolić: Age is the most important factor. From the mid-30s onwards, egg quality declines noticeably, and from the age of 40 onwards, the risk of chromosomal changes increases significantly. This has a direct impact on the chances of pregnancy.
What can women do themselves to improve or positively influence their egg quality?
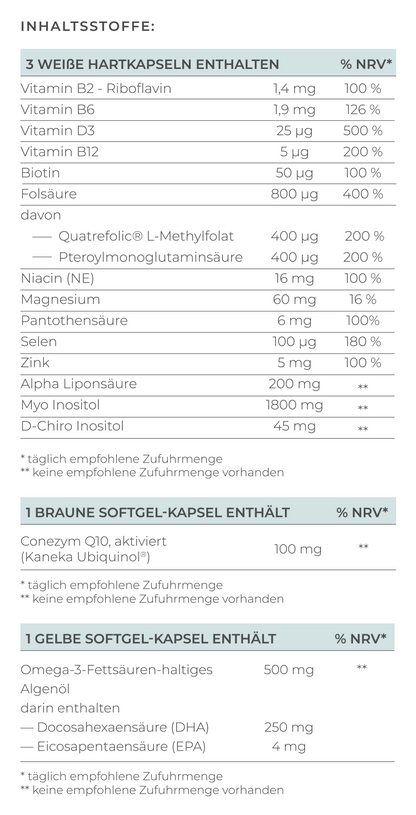
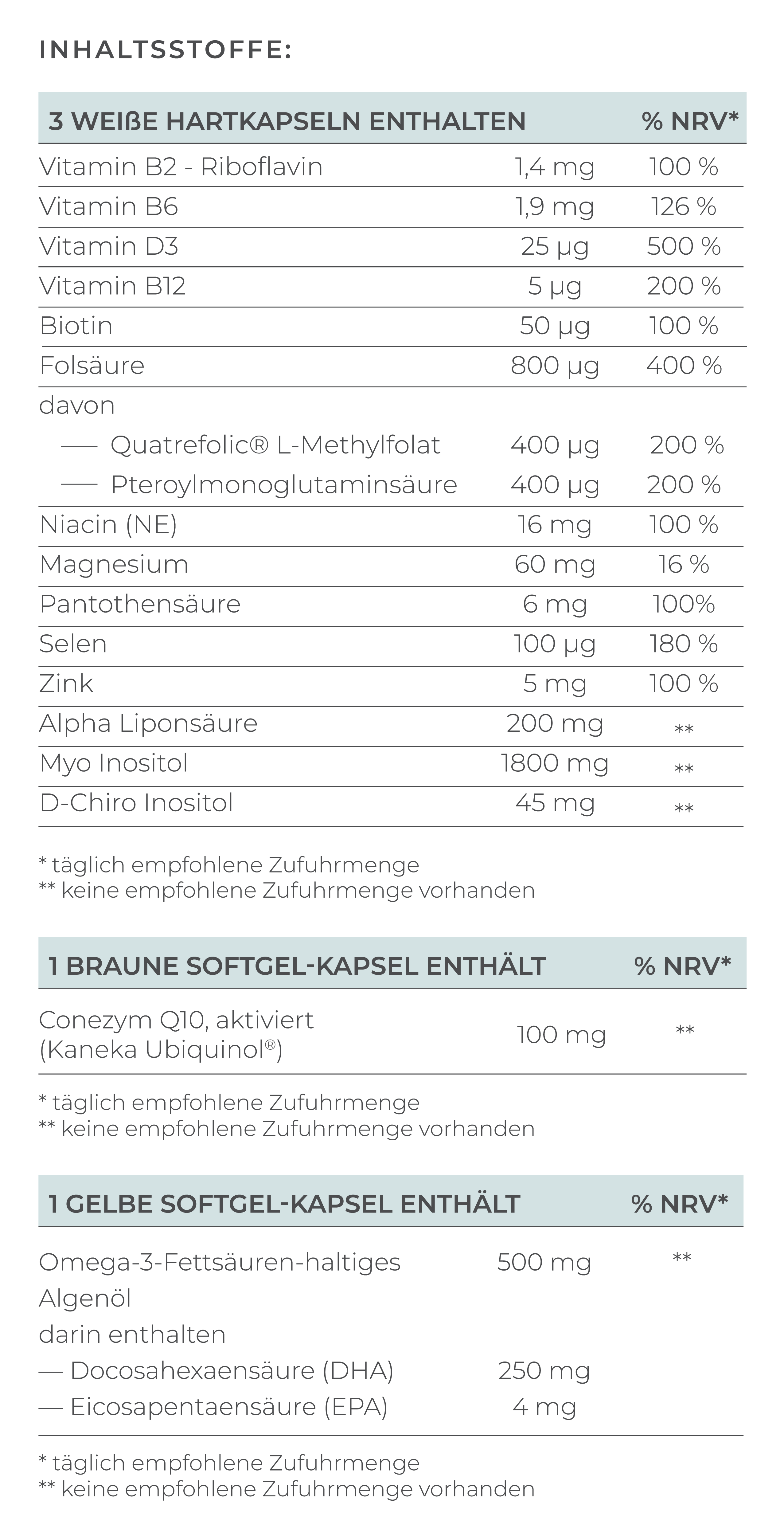
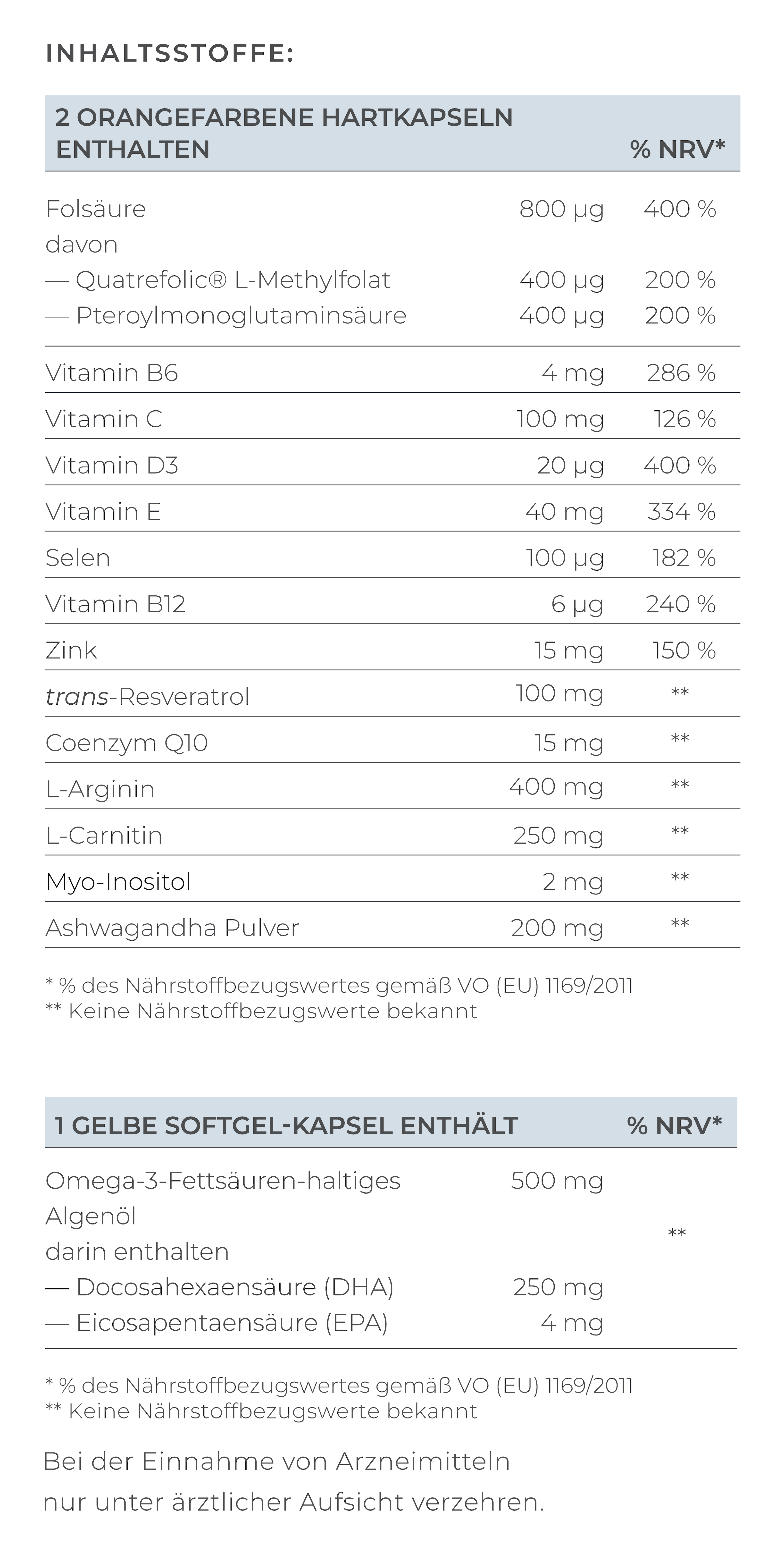
Nenad Nikolić: We cannot stop the natural decline, but women can do a number of things: sticking to a healthy diet, no smoking, drinking little alcohol, getting enough sleep, and exercising. Stress reduction also plays an important role. Certain micronutrients such as antioxidants or omega-3 fatty acids can also be helpful – in consultation with a doctor, of course.
And what can a man do to improve his sperm quality?
Nenad Nikolić: Basically, the same applies here. Avoiding smoking and the consumption of alcohol, sticking to a balanced diet, losing excess weight, and exercising regularly. It is also important to avoid overheating the testicles, for example, by not placing laptops directly on your lap or going to the sauna all the time. In addition, zinc, selenium, or vitamin C and E can have a supportive effect on male fertility.
Can you explain what exactly happens in the laboratory after the eggs and sperm have been collected?
Nenad Nikolić: Once the eggs and sperm have been retrieved, the procedures differ depending on the method used. In classic IVF, the eggs remain enclosed in their surrounding cells and are placed in culture together with processed sperm so that fertilization can occur naturally. In ICSI, on the other hand, we remove the eggs from these surrounding cells so that we can accurately assess their maturity, and then inject a single sperm directly into the egg. Regardless of the method, the fertilized eggs are then cultured in special incubators.
How do you assess the quality of embryos—what do you pay particular attention to?
Nenad Nikolić: We pay particular attention to the division rate, the uniformity of the cells, and the degree of fragmentation. A good embryo divides regularly and has uniform, clear structures with few fragments.
What criteria are used to classify embryos, and what constitutes good embryo quality?
Nenad Nikolić: On day 3, we look at the cell count, symmetry, and fragmentation—6 to 10 uniform cells are optimal. For blastocysts on day 5 or 6, we evaluate the inner cell mass and trophectoderm as well as the size of the fluid cavity. A good blastocyst shows clear structures and balanced development.
What does it mean when an embryo is a “blastocyst”? Why is this often a good sign?
Nenad Nikolić: A blastocyst is an embryo that has reached this blastocyst stage five or six days after fertilization. The fact that it has progressed this far shows that it has high development potential. Blastocysts therefore have a higher chance of implanting in the uterus.
How do day 3 embryos differ from blastocysts in terms of quality and transfer?
Nenad Nikolić: Day 3 embryos consist of a few cells, whereas blastocysts consist of hundreds. With a blastocyst culture, we can identify more accurately which embryos have the best potential. However, not all embryos make it to day 5. Therefore, the decision is individual and depends on the patient's situation.
If several embryos develop well, how do you decide which embryo to transfer?
Nenad Nikolić: We combine morphological criteria, i.e., the appearance of the embryo, with dynamic data, for example, from time-lapse monitoring. In addition, we consider the medical conditions and the individual situation of the patient. Ultimately, we select the embryo with the highest implantation potential.
What role does the ICSI method play in cases of limited sperm quality, and how does this affect embryo development?
Nenad Nikolić: ICSI is a tremendous help when sperm quality is very limited. The method has no disadvantages for embryo development itself—the key is that we select healthy sperm.
What is time-lapse monitoring, and how does this technology help you select the best embryo?
Nenad Nikolić: Time-lapse means that embryos are continuously recorded in special incubators. This allows us to see their development from fertilization to blastocyst in real time without removing them from the incubator. This is a major advantage because the culture conditions remain stable—there are no influences from light, pH changes, or temperature fluctuations. In addition, continuous observation allows us to detect subtle differences in the division pattern, which helps us to select the embryo with the best potential.
How important is the collaboration between you as an embryologist and the medical team for the success of the treatment?
Nenad Nikolić: It is absolutely crucial. We work closely with the treating physicians—from stimulation planning to embryo transfer. Only when we bring all the information together can we make the best individual decision for the patient.
What new developments or technologies do you see that could further improve embryo assessment in the future?
Nenad Nikolić: I think artificial intelligence will play a major role. There are already systems that analyze embryos based on images and calculate the probabilities of implantation. Genetic tests are also becoming increasingly accurate. The goal is to make the selection of the best embryo as objective and reliable as possible.